Imported Mansonella perstans infection in Spain - Infectious Diseases of Poverty - Infectious Diseases of Poverty - BioMed Central
Demographic and epidemiological data
In total, 503 cases of M. perstans infection were identified at the Carlos III Hospital. The main epidemiological data are shown in Table 1. Two hundred sixty-four patients were female (52.5%). The migrants' mean age (±SD) was 44.6 ± 18.2 years (range: 16–93); the median (25th, 75th percentiles) age was 43 years (28, 60). Most of them (97.6%) came from Equatorial Guinea, 12 cases came from other African countries: D.R.Congo (3), Cameroon (2), Guinea Bissau (2), Nigeria (2), Gabon (1), Guinea Conakry (1) and Togo (1). All the patients were infected in their country of origin. The mean time (± SD) between their arrival to Spain and their first medical consultation was 8.6 ± 18.0 months (range: 1–180); the median (25th, 75th percentiles) time was 2 months (1, 7). Half of the patients (50.3%) were evaluated during the first month of stay in Spain. The mean number of cases (± SD) was 25.1 ± 11.8 (5–45) per month, with an irregular chronological distribution.
Clinical and laboratory data
The main clinical and analytical patient data are described in Table 1, according to the variables "Microbiological association", Mansonella perstans (n1 = 308, 61.2%) vs coinfections (n2 = 195, 38.8%) and "Clinical association", symptomatic (n3 = 228, 45.3%) vs asymptomatic (n4 = 275, 54.7%). Clinical manifestations were observed in 228 patients (45.3%). The most frequent symptom was pruritus in 190 patients (83.3%), arthralgia in 50 patients (9.9%), abdominal pain in 15 patients (3.0%) and Calabar swelling in 18 patients (3.6%). Significant differences (P = 0.010) were found between the percentage of males with symptoms (41.2%) and females with symptoms (58.8%), and no significant differences in age were found (P = 0.771).
Regarding eosinophilia levels, 105 (20.9%) patients had a normal eosinophil count, 58 (11.5%) had relative eosinophilia and 340 (67.6%) patients had absolute eosinophilia: mild eosinophilia in 159 patients (31.6%), moderate eosinophilia in 154 patients (30.6%) and severe eosinophilia in 27 patients (5.4%). Moreover, 152/228 (66.6%) symptomatic patients had absolute eosinophilia vs 188/275 (68.3%) asymptomatic patients. Statistically significant differences were found between the percentages of symptomatic vs asymptomatic cases and levels of eosinophilia (P < 0.001). Concerning IgE detection, 49 (10%) patients had normal levels, and the remainder (442, 90%) had hyper-IgE: mild hyper-IgE (57, 11.6%), moderate hyper-IgE (105, 21.4%) and severe hyper-IgE (280, 55.7%). No statistically significant differences were found between asymptomatic and symptomatic patients and IgE (P = 0.749). Finally, 240 (47.7%) cases healed. Among the remaining 263 (52.3%) cases, 245 (48.7%) individuals had no follow-up data and 18 (3.6%) cases were not cured.
Microbiology data
The microorganism coinfection in patients with Mansonella perstans infection showed in Table 2. Globally, 308 migrants (61.2%) had only M. perstans infections and 195 patients (38.8%) had coinfection with other filarial nematodes. Onchocerca volvulus was the most frequent filarial coinfection with 138 patients (27.4%). One hundred eighty-six patients (37%) had coinfection with other helminths. Trichuris trichiura was the most frequent helminthic coinfection, with 137 patients (27.2%). Moreover, 73 (14.5%) patients presented simultaneously with other filarial and helminthic coinfections. Additionally, 78 patients (15.5%) were protozoa coinfected, mainly with amoebas (58, 11.5%). Finally, 26 patients (5.2%) had HIV coinfection.
The presence of coinfections was not significantly related to gender (48.4% males vs 51.6% females, P = 0.627). No significant differences were found between age groups (P = 0.228). By contrast, a higher percentage of patients infected only with M. pertans was asymptomatic (63%) than patients coinfected (58.5%) (P < 0.001). Coinfected patients had higher absolute eosinophilia percentages (P < 0.001), severe eosinophilia (10.8% vs 1.9%) and moderate eosinophilia (40.5% vs 24.4%). Similarly, coinfected patients had higher hyper-IgE, severe and moderate (P = 0.001) (see Table 1).
Treatment and outcome
Four hundred thirty-seven cases (86.9%) were treated, 66 (13.1%) cases were untreated, and 292 cases (58.1%) used only one drug: mebendazole 100 mg/12 h/30 days (n = 267), ivermectin 200 μg/kg single dose (n = 16) and albendazole 400 mg/12 h/3 weeks (n = 9). By contrast, 145 cases (28.8%) used combined therapy, mainly ivermectin and mebendazole (n = 113), as shown in Table 3. Therefore, the drug most used, alone or associated, was mebendazole, in 407 patients. Most of them (n = 382) received a single course, 24 double courses and 1 triple courses. Corticosteroid therapy was administered concurrently with the anti-filarial drug in 20 (4%) cases, and an antihistaminic drug was administered with the anti-filarial drug in 38 (7.6%) cases. Figure 1 shows a significant decrease in eosinophilia before and after treatment (P < 0.001).
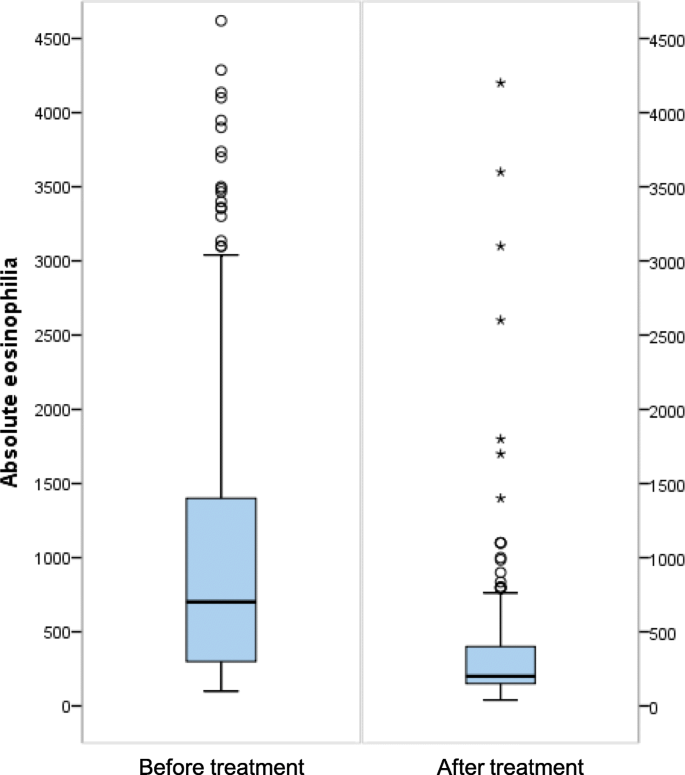
Eosinophilia before and after treatment
Adverse reactions to the anti-filarial drugs occurred in 25 (5%) migrants: 15 had pruritus (13 associated with mebendazole and 2 with ivermectin), 3 had pruritus and skin abscess (3 mebendazole), 1 had arthritis (dietilcarbamazine and ivermectin and mebendazole), and 1 had hepatotoxicity (diethylcarbamazine [DEC] and albendazole).
Comments
Post a Comment