Eating Disorders Among Older Adults - Psychiatric Times

Photographee.eu/AdobeStock

CATEGORY 1 CME
Premiere Date: February 20, 2023
Expiration Date: August 20, 2024
This activity offers CE credits for:
1. Physicians (CME)
2. Other
All other clinicians either will receive a CME Attendance Certificate or may choose any of the types of CE credit being offered.
ACTIVITY GOAL
The goal of this activity is to learn how to evaluate older adults who present with significant appetite and weight changes for the presence of an eating disorder.
LEARNING OBJECTIVES
1. Describe the epidemiology of eating disorders among older adults.
2. Discuss the evidence-based assessment and management of eating disorders among older adults.
TARGET AUDIENCE
This accredited continuing education (CE) activity is intended for psychiatrists, psychologists, primary care physicians, physician assistants, nurse practitioners, and other health care professionals seeking to improve the care of patients with mental health disorders.
ACCREDITATION/CREDIT DESIGNATION/FINANCIAL SUPPORT
This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint providership of Physicians' Education Resource®, LLC, and Psychiatric Times™. Physicians' Education Resource®, LLC, is accredited by the ACCME to provide continuing medical education for physicians.
Physicians' Education Resource®, LLC, designates this enduring material for a maximum of 1.5 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
This activity is funded entirely by Physicians' Education Resource®, LLC. No commercial support was received.
OFF-LABEL DISCLOSURE/DISCLAIMER
This accredited CE activity may or may not discuss investigational, unapproved, or off-label use of drugs. Participants are advised to consult prescribing information for any products discussed. The information provided in this accredited CE activity is for continuing medical education purposes only and is not meant to substitute for the independent clinical judgment of a physician relative to diagnostic or treatment options for a specific patient's medical condition. The opinions expressed in the content are solely those of the individual faculty members and do not reflect those of Physicians' Education Resource®, LLC.
FACULTY, STAFF, AND PLANNERS' DISCLOSURES AND CONFLICT OF INTEREST (COI) MITIGATION
The staff members of Physicians' Education Resource®, LLC, and Psychiatric Times™ and the authors have no relevant financial relationships with commercial interests.
None of the staff of Physicians' Education Resource®, LLC, or Psychiatric Times™ or the planners of this educational activity have relevant financial relationship(s) to disclose with ineligible companies whose primary business is producing, marketing, selling, reselling, or distributing health care products used by or on patients. Drs Tampi and Tampi note they have nothing to disclose regarding this article.
For content-related questions, email us at PTEditor@mmhgroup.com. For questions concerning the accreditation of this CE activity or how to claim credit, please contact info@gotoper.com and include "Eating Disorders Among Older Adults" in the subject line.
HOW TO CLAIM CREDIT
Once you have read the article, please use the following URL to evaluate and request credit: https://education.gotoper.com/activity/ptcme23feb. If you do not already have an account with Physicians' Education Resource®, LLC, you will be prompted to create one. You must have an account to evaluate and request credit for this activity.
The DSM-5 describes eating disorders (EDs) as conditions that are characterized by a persistent disturbance of eating or eating-related behaviors.1 These disorders result in an altered consumption or absorption of food that causes a significant impairment in physical health or psychosocial functioning. The DSM-5 identifies 8 different types of EDs: pica, rumination disorder, avoidant/restrictive food intake disorder, anorexia nervosa (AN), bulimia nervosa (BN), binge-eating disorder (BED), other specified feeding or eating disorder, and unspecified feeding or eating disorder.
The diagnostic criteria for these 8 disorders result in a classification scheme that identifies mutually exclusive disorders.1 As a result, an individual can only be assigned 1 of these diagnoses during a single episode. According to the DSM-5, the classification is necessary because these are heterogenous disorders that have considerably different clinical courses, outcomes, and treatment needs. An exception to this rule is the diagnosis of pica, which may be assigned with any of the other eating disorders. The DSM-5 does not consider obesity to be an ED.
Epidemiology
A recent systematic review and meta-analysis by Qian et al found the pooled lifetime and 12-month prevalences of EDs to be 0.91% and 0.43%, respectively.2 The lifetime prevalences of AN, BN, and BED were 0.16%, 0.63%, and 1.53%, respectively. The investigators also found that the lifetime prevalence of EDs in Western countries was 1.89% in men and 2.58% in women. An earlier systematic review had found that the point prevalence was 5.7% for women and 2.2% for men; the 12-month prevalence was 2.2% for women and 0.7% for men; and the lifetime prevalence was 8.4% for women and 2.2% for men.3 The authors also noted that the point prevalence of EDs in North America was 4.6%, compared with 2.2% in Europe and 3.5% in Asia.
Although the exact prevalence of EDs among older adults is unclear, a survey conducted by Mangweth-Matzek et al of community-dwelling women aged 60 to 70 years found that 3.8% of the participants met the criteria for an ED.4 In another study that included a nationally representative sample of women 50 years and older, Gadalla found that approximately 2.6% of women aged 50 to 64 years and 1.8% of women 65 years and older reported disordered eating symptomatology.5
Similarly, Mangweth-Matzek et al found that among Canadian women aged 40 to 60 years, 4.6% of individuals met the full DSM-IV criteria for an ED, whereas an additional 4.8% met the subthreshold criteria for an ED.6 In this study, BED (33%) and BN (30%) were the most common ED diagnoses.
A literature review by Lapid et al found a total of 48 published cases of EDs among individuals 50 years and older.7 In this review, 88% of the cases involved women; 40% of the cases were among individuals aged 50 to 64 years and 60% of the cases involved individuals 65 years and older. In addition, the authors noted that AN (81%) and BN (10%) were the most common ED diagnoses. AN (83%) was the most common ED diagnosis in women followed by BN (10%). Among men, AN (67%) was the most common ED, followed by BN (17%). In this study, 69% of the individuals had a late-onset ED, with 58% having onset between age 45 to 62 years and 33% of individuals having the onset of an ED after age 65 years.
In a systematic review of literature of 39 cases of EDs among individuals 65 years and older, the majority of individuals were women (84.6%) and AN (84.6%) was the most common diagnosis.8 BN was seen in only 7.7% of the cases. Among women, AN (87.9%) was the most common ED, followed by BN (6.1%). Among the men, AN (66.7%) was the most common diagnosis, followed by BN (16.7%). In this review, the investigators found that 56.4% of all cases had late-onset EDs (after age 40 years).
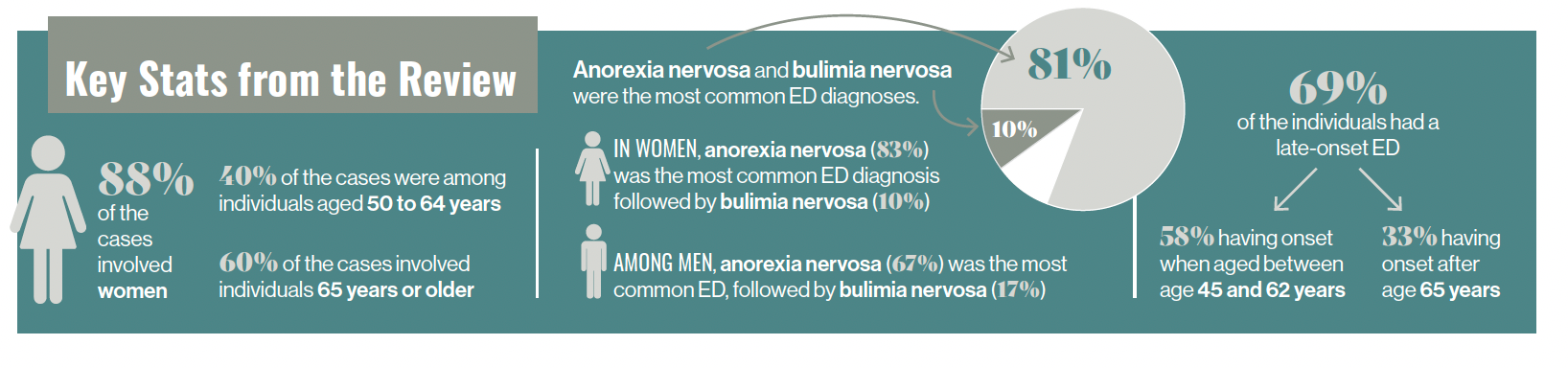
Key Stats from the Review
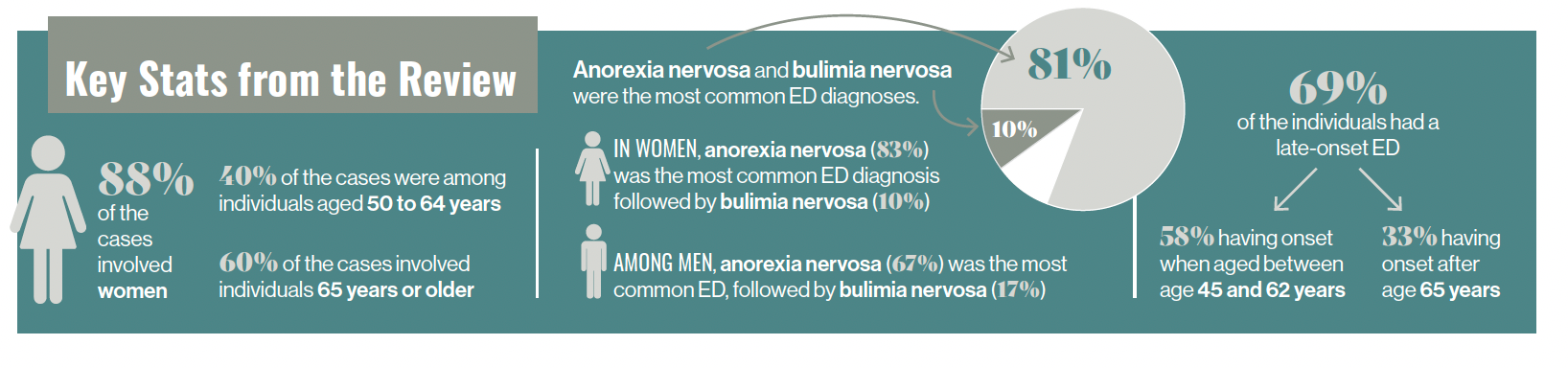
Lapid et al found that 69% of individuals had a late-onset ED in their sample, but they have been challenged by other authors who opine that most cases of EDs are carried over into older age from an onset in younger age.9 Aziz et al opined that older adults with EDs belong to 1 of 3 categories: (1) individuals who develop an ED in early adulthood and have a chronic condition that continues into older age; (2) individuals who develop an ED in young adulthood, are treated, but have a recurrence of symptoms in older age; and (3) older adults who develop an ED for the first time later in life.10 The third category of individuals with EDs is the rarest. However, there may be a fourth category composed of individuals who have had symptoms of disordered eating for many years that have never met the criteria for any formal ED diagnosis (subclinical ED), but during periods of high stress and life changes, the symptoms of ED worsen and they now meet the formal diagnostic criteria for an ED at an older age. Some of the individuals who develop EDs for the first time at an older age likely include individuals from the fourth category. Common stressors that result in the onset or recurrence of EDs in older individuals include the losses of friends and family, traumatic illness, divorce/remarriage, and empty nest syndrome.11 It is possible that approximately one-third of all ED cases have their onset at an older age, versus two-thirds at a younger age.12
Based on the available evidence, it can be inferred that EDs appear less prevalent among older adults than younger adults.4-11 However, these data may be influenced by significant underreporting of cases of EDs among older adults. Additionally, the symptoms of EDs among older adults may often be misattributed to or masked by other medical or psychiatric disorders. Among the EDs seen in older adults, AN appears to be the most common, followed by BN. EDs also appear more common among older women than older men.
Differences in Onset
Compared with individuals with typical-onset EDs, older individuals with EDs have more marital conflicts, separation, or divorce; however, they are less likely to have a family history of major psychiatric disorders and an occurrence of comorbidities (with the exception of anxiety and depression).13 Older individuals with EDs also present with a more frequent history of past or current obesity compared with younger individuals with EDs. These individuals also present with fewer vomiting episodes and self-harming behaviors, but they have greater rates of purging episodes using laxatives.14
Older individuals also appear to have a greater prevalence of comorbid depression and anxiety compared with younger individuals with EDs.13 Prevalence of substance use disorders and obsessive-compulsive personality disorders are the same among older adults and younger patients. Despite the risk of medical complications being similar between the 2 groups, the risk of morbidity and mortality due to gastric, bone, metabolic, and cardiovascular disorders is higher among older adults with EDs.
Examining Comorbidities
A secondary data analysis of the Canadian Community Health Survey evaluated the risk of mood disorders, anxiety disorders, and alcohol dependence among individuals with ED symptomatology as compared with individuals without ED symptomatology in community-dwelling women aged 50 years and older.5 The investigators found increased risk of mood disorders in women with ED symptomology. Compared with women without ED symptomatology, the odds of having a mood disorder were 6.9 times higher for women aged 50 to 64 years (P < .0005) and 3.2 higher for women 65 years and older (P < .05) for those with symptomology. Additionally, the odds of having anxiety disorders in women with ED symptomatology were 2.6 times higher for women aged 50 to 64 years (P< .005) and 5.6 times higher for women 65 years and older (P < .0005), compared with women who had no ED symptomatology. Furthermore, the odds of alcohol dependency for women aged 50 to 64 years with ED symptomatology was 6.0 times higher compared with women who had no ED symptomatology (P < .05). This survey did not identify alcohol dependence among any woman 65 years or older.
In their review, Lapid et al found comorbid psychiatric disorders or a previous history of psychiatric disorders in 60% of the individuals with EDs.7 The most common psychiatric disorder was major depression (69%). Similarly, Mulchandani et al found that 54% of individuals with EDs had a comorbid psychiatric diagnosis; 31% had comorbid depression. Anxiety, schizophrenia/schizoaffective disorder, and dementia were also common comorbidities, with each represented in 5% of the individuals.8
Etiologies
Medical disorders, psychiatric disorders, and social factors can precipitate or worsen EDs among older adults.10,15 Medical causes include a loss of taste or smell, dry mouth, poor oral and dental hygiene, problems with dentures, pain, gastroesophageal reflux disease, diabetes, and polypharmacy. Depression and dementia are among the psychiatric causes of disordered eating. Eating difficulties in patients with dementia often tend to occur during the moderate-to-severe stages of the disease. Isolation, financial difficulties, inability to obtain or cook food due to physical or cognitive limitations, lack of caregivers, and elder abuse are some of the social factors that can precipitate EDs in this patient population.
Concerns with an aging physical appearance are also related to the development of EDs, with a direct correlation between concerns about an aging appearance and the drive for thinness and excessive dieting.16 One study of community-dwelling women aged 40 to 60 years found that perimenopausal women had significantly greater prevalence of EDs and body image pathology compared with premenopausal women.17 This study also found that women with surgically induced menopause showed an elevated prevalence of eating and body image pathology. The investigators opined that just like puberty, menopause represents a window of vulnerability for developing EDs due to changes in hormonal functions, body composition, and concepts of womanhood.
A need for control or attention may also be a psychological factor. For instance, an individual's disordered eating may come from an attempt to gain control in their life or to get the attention of loved ones during stressful times or periods of personal uncertainty.11 A study of middle-aged women found that risk factors for lifetime EDs include childhood sexual abuse, unhappiness, and low parental care.18 The authors also postulated that high interpersonal sensitivity, which is described as the sensitivity to others' feedback and the fear of social rejection, might also contribute to the onset and maintenance of EDs.
Emerging evidence primarily indicates that EDs among older individuals are likely to be biologically based illnesses with psychological and social factors acting as predisposing, precipitating, and perpetuating factors.10-18 As among younger adults, many older individuals "diet" or intentionally limit intake, but only a very small percentage of these individuals develop actual EDs.
Outcomes
Although not specific to older patients, available evidence indicates that individuals with EDs have greater rates of morbidity and mortality than age-matched controls and the general population. A meta-analysis by Arcelus et al found that the weighted mortality rates (deaths per 1000 person-years) were 5.1 for AN, 1.7 for BN, and 3.3 for other EDs.19 This study also found that 1 in 5 individuals with AN had suicided.
Similarly, in an electronic health records study, individuals with EDs had greater rates of other mental disorders (odds ratio [OR], 4.32) as well as external causes of morbidity and mortality (OR, 2.92), compared with age-matched controls.20 In addition, individuals with EDs also had greater prescription of central nervous system drugs (OR, 3.15), gastrointestinal drugs (OR, 2.61), and dietetic drugs (OR, 2.42) prior to the diagnosis.
Specifically, mortality rates were high among individuals with AN, with 6% deceased within 15 years of the diagnosis. Individuals with AN were more likely to die than controls (hazard ratio [HR], 2.33); this was especially true for women with AN (HR, 2.53). Mortality was also slightly higher for individuals with BN (HR, 1.41) and other EDs (HR, 1.82) compared with controls. The most common reasons for death among individuals with ED were respiratory disorders (17.9% of deaths); followed by injury, poisoning, and certain other consequences of external causes (13.3% of death); and diseases of the digestive system (11.4% of deaths). Evidence indicates that the mortality risk for individuals with AN who have received inpatient treatment is more than 5 times greater than for those who have not received this treatment, probably indicating that this group includes individuals with more severe illness.
Morbidity is also an issue, as studies indicate patients have a reduced quality of life and 48% greater annual health care costs compared with the general population.21 For example, in the Lapid et al review, although 42% of the individuals saw an improvement in symptoms and/or gained weight, 20% of the individuals died as a result of their EDs or their complications.7 Similarly, Mulchandani et al found that 67% of the individuals with AN had an improvement in symptoms, but nearly a quarter (24.2%) had either relapsed or died. Interestingly, all of the individuals with BN saw an improvement in symptoms and were still alive.8
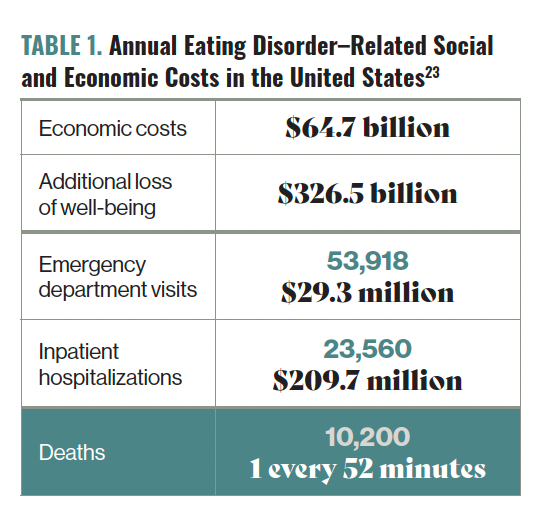
Table 1. Annual Eating Disorder–Related Social and Economic Costs in the United States23
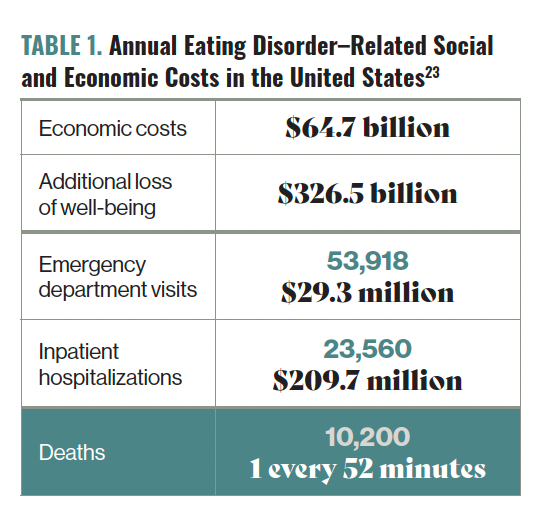
The morbidity and mortality associated with EDs impact patients and the community. Table 1 highlights the social and economic costs of EDs in the United States.22
Assessment
Diagnosing EDs in older adults can often be difficult, as aging in itself can result in changes in appetite and weight.10 Many of these individuals also have underlying medical and/or psychiatric disorders that can alter their appetite and cause changes in weight. Because EDs, especially AN, have a high mortality rate among older adults, a prompt and detailed assessment should occur once an ED diagnosis is suspected.7 A comprehensive history, a thorough mental status examination including cognitive assessment, focused physical examination, and appropriate laboratory workup will assist with identifying confounding medical and psychiatric disorders that are associated with changes in appetite, eating habits, and weight.7
Getting information from collateral sources (eg, family members) is important to establish a timeline for the development of the disorder. A history of EDs should also be assessed, as many older adults have a history of EDs starting in their late teens or early adulthood. Although there are no specific screening tools for EDs among older adults, the Sick, Control, One, Fat, Food (SCOFF) questionnaire can be used.7 Among adults, the SCOFF has a sensitivity of 0.86 and specificity of 0.83.23
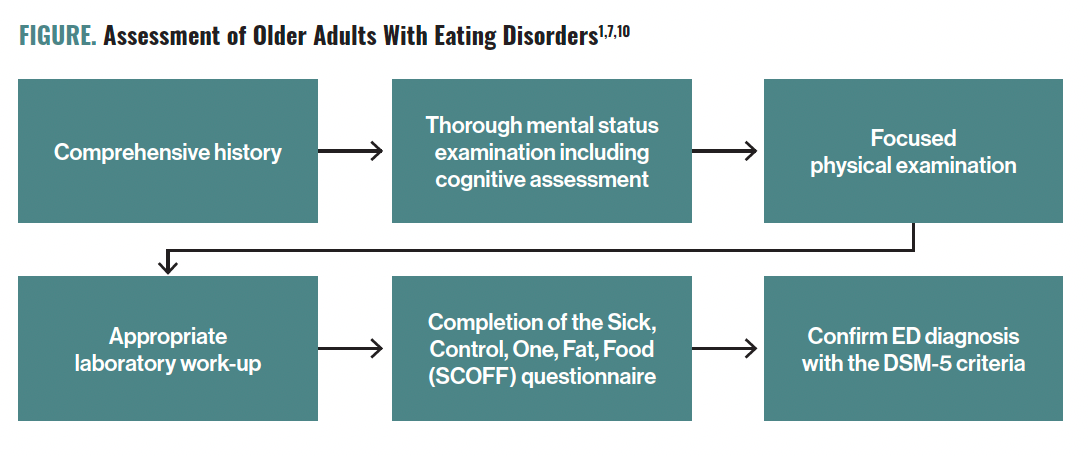
Figure. Assessment of Older Adults With Eating Disorders1,7,10
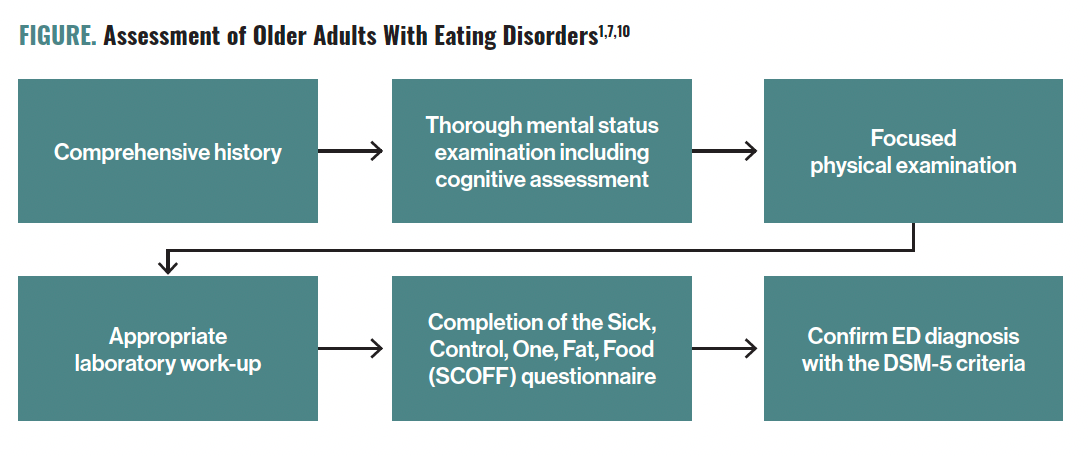
Common medical and psychiatric disorders that can present with symptoms of EDs among older adults include hypothyroidism, depression, psychosis, and dementias.10 On physical examination, being underweight as well as having anemia, low temperature, bradycardia, hypotension, and hair loss may indicate a diagnosis of AN, whereas dental erosion, edema, salivary gland hypertrophy, and lesions of dorsum of hands (Russell's sign) may indicate BN.7 The Figure describes the evidence-based assessment of older adults with EDs.
Treatments
Available evidence indicates inconsistency in the treatment of EDs among older adults, possibly due to lack of awareness of these disorders and their treatments.8 However, current evidence also indicates that treatments for older adults are very similar to those for younger individuals.7 Although limited, available data indicate that multimodal treatment approaches, including a combination of psychotherapy and pharmacotherapy, show the greatest benefit in older individuals with EDs.7,8
Additionally, a dietician can assist with nutritional rehabilitation, in which the goal is for the individual to gain weight.7 It is also prudent to involve close family members in treatment planning and to encourage them to take an active role in helping the patient first gain and then maintain weight. Given the significant potential negative outcomes, older patients should have close follow-up to ensure adherence to treatment and to intervene quickly in cases where their health and well-being are compromised. Cognitive behavioral therapy (CBT), interpersonal therapy (IPT), and psychodynamic and family therapy have all shown benefit in the treatment of older adults with ED.7 Limited data exist for the use of psychotropic medications among older adults with EDs, although antidepressants, anxiolytics, and antipsychotic medications (especially olanzapine) may show benefit when used in combination with psychotherapies.7,8 Fluoxetine has been FDA approved for acute treatment and maintenance of BN since 1994 and lisdexamfetamine was approved by the FDA in 2015 for the maintenance treatment of moderate-to-severe BED.24
Although not specific to older adults, a comparison of evidence-based clinical international guidelines found many consistent recommendations.25
For the treatment of AN, family-based therapy was found to be beneficial for younger individuals. Additionally, benefits were noted for CBT, the Maudsley Anorexia Nervosa Treatment for Adults, and Specialist Supportive Clinical Management. There was little agreement among the guidelines for IPT and psychodynamic psychotherapy as alternative treatments. The careful use of antipsychotics was noted to reduce associated obsessional thinking among individuals with AN. Some guidelines recommended antidepressants for the treatment of depressive symptoms, but there was no consistent recommendation for any specific type of antidepressant.
For the treatment of BN, CBT was found to be beneficial, with IPT as an alternative to CBT. Most guidelines also recommended guided CBT self-help treatment. Limited evidence was noted for nutritional counseling and the combination of psychodynamic psychotherapy and CBT.
Most guidelines recommended the use of antidepressants (especially fluoxetine) for the treatment of BN to be used only in combination with psychotherapy.
For the treatment of BED, CBT was found to be beneficial. Guided CBT self-help treatment and IPT were also found to be beneficial among individuals with BED. For the pharmacological treatment of BED, the use of selective serotonin reuptake inhibitors was found to be beneficial.
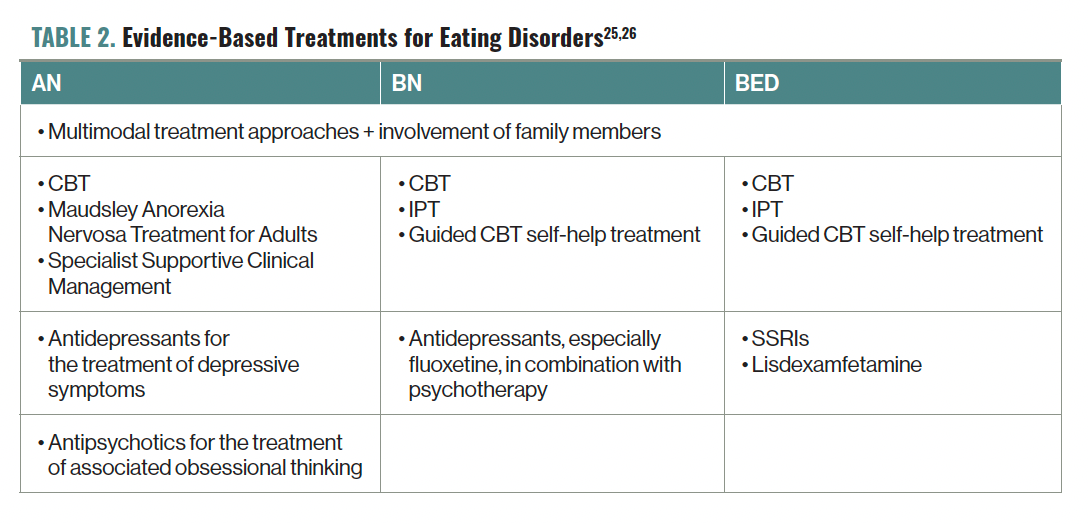
Table 2. Evidence-Based Treatments for Eating Disorders25,26
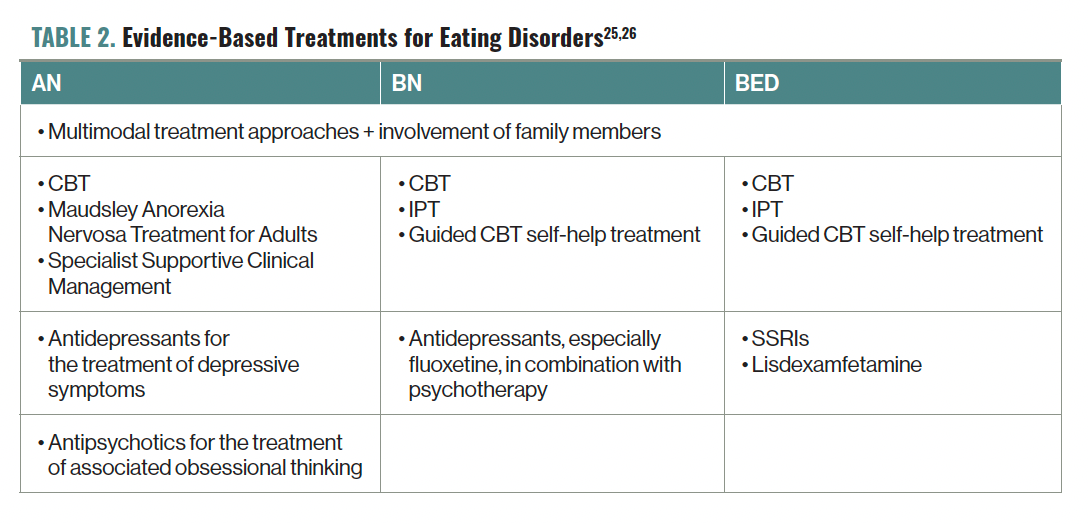
Table 2 describes the evidence-based treatments for EDs among adults; these could also be adapted for use among older adults with EDs.
Concluding Thoughts
EDs are not uncommon among older adults. The majority of cases are in individuals who experienced early onset of an ED (ie, when they were younger). As a result, there are many commonalities between the courses and treatments of EDs in older and younger patients. For instance, medical disorders, psychiatric disorders, and social factors can precipitate or worsen EDs among older adults. Psychiatric comorbidities are also common among older adults with EDs. The occurrence of EDs among older adults is associated with significant rates of morbidity and mortality. Mortality rates are significantly higher among older individuals with AN compared with other EDs.
When EDs are suspected among older adults, a prompt and thorough evaluation with swift initiation of treatment are crucial steps in minimizing the morbidity and mortality that can be associated with these serious illnesses. Once an ED is identified, multimodal treatment approaches that include both psychotherapy and pharmacotherapy have been shown to offer the greatest benefit. Future studies should include individuals from varied cultural and ethnic backgrounds, along with the use of the latest diagnostic criteria to correctly identify these disorders.
Dr Tampi is professor and chairman of the Department of Psychiatry at Creighton University School of Medicine and Catholic Health Initiatives Health Behavioral Health Services in Omaha, NE. He is also an adjunct professor of psychiatry at Yale School of Medicine. Ms Tampi is cofounder and managing principal of Behavioral Health Advisory Group in Princeton, NJ.
References
1. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. American Psychiatric Association; 2013.
2. Qian J, Wu Y, Liu F, et al. An update on the prevalence of eating disorders in the general population: a systematic review and meta-analysis. Eat Weight Disord. 2022;27(2):415-428.
3. Galmiche M, Déchelotte P, Lambert G, Tavolacci MP. Prevalence of eating disorders over the 2000-2018 period: a systematic literature review. Am J Clin Nutr. 2019;109(5):1402-1413.
4. Mangweth-Matzek B, Rupp CI, Hausmann A, et al. Never too old for eating disorders or body dissatisfaction: a community study of elderly women. Int J Eat Disord. 2006;39(7):583-586.
5. Gadalla TM. Eating disorders and associated psychiatric comorbidity in elderly Canadian women. Arch Womens Ment Health. 2008;11(5-6):357-362.
6. Mangweth-Matzek B, Hoek HW, Rupp CI, et al. Prevalence of eating disorders in middle-aged women. Int J Eat Disord. 2014;47(3):320-324.
7. Lapid MI, Prom MC, Burton MC, et al. Eating disorders in the elderly. Int Psychogeriatr. 2010;22(4):523-536.
8. Mulchandani M, Shetty N, Conrad A, et al. Treatment of eating disorders in older people: a systematic review. Syst Rev. 2021;10(1):275.
9. Main J, Reddy L, Lazarevic M, Whelan PJ. Are late-onset eating disorders in the elderly really the more common variant? Concerns around publication bias. Int Psychogeriatr. 2011;23(4):670-671.
10. Aziz VM, Rafferty D, Jurewicz I. Disordered eating in older people: some causes and treatments. BJPsych Advances. 2017;23(5):331-337.
11. Harris M, Cumella EJ. Eating disorders across the life span. J Psychosoc Nurs Ment Health Serv. 2006;44(4):20-26.
12. Mangweth-Matzek B, Hoek HW, Pope HG Jr. Pathological eating and body dissatisfaction in middle-aged and older women. Curr Opin Psychiatry. 2014;27(6):431-435.
13. Luca A, Luca M, Calandra C. Eating disorders in late-life. Aging Dis. 2014;6(1):48-55.
14. Bueno B, Krug I, Bulik CM, et al. Late onset eating disorders in Spain: clinical characteristics and therapeutic implications. J Clin Psychol. 2014;70(1):1-17.
15. Landi F, Calvani R, Tosato M, et al. Anorexia of aging: risk factors, consequences, and potential treatments. Nutrients. 2016;8(2):69.
16. Gupta MA. Concerns about aging and a drive for thinness: a factor in the biopsychosocial model of eating disorders? Int J Eat Disord. 1995;18(4):351-357.
17. Mangweth-Matzek B, Hoek HW, Rupp CI, et al. The menopausal transition--a possible window of vulnerability for eating pathology. Int J Eat Disord. 2013;46(6):609-616.
18. Micali N, Martini MG, Thomas JJ, et al. Lifetime and 12-month prevalence of eating disorders amongst women in mid-life: a population-based study of diagnoses and risk factors. BMC Med. 2017;15(1):12.
19. Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders. A meta-analysis of 36 studies. Arch Gen Psychiatry. 2011;68(7):724-731.
20. Demmler JC, Brophy ST, Marchant A, et al. Shining the light on eating disorders, incidence, prognosis and profiling of patients in primary and secondary care: national data linkage study. Br J Psychiatry. 2020;216(2):105-112.
21. van Hoeken D, Hoek HW. Review of the burden of eating disorders: mortality, disability, costs, quality of life, and family burden. Curr Opin Psychiatry. 2020;33(6):521-527.
22. Strategic Training Initiative for the Prevention of Eating Disorders, Academy for Eating Disorders, Deloitte Access Economics. Social & economic cost of eating disorders in the United States. Harvard T.H. Chan School of Public Health. June 2020. Accessed November 24, 2022. https://www.hsph.harvard.edu/striped/report-economic-costs-of-eating-disorders/
23. Kutz AM, Marsh AG, Gunderson CG, et al. Eating disorder screening: a systematic review and meta-analysis of diagnostic test characteristics of the SCOFF. J Gen Intern Med. 2020;35(3):885-893.
24. Bello NT, Yeomans BL. Safety of pharmacotherapy options for bulimia nervosa and binge eating disorder. Expert Opin Drug Saf. 2018;17(1):17-23.
25. Hilbert A, Hoek HW, Schmidt R. Evidence-based clinical guidelines for eating disorders: international comparison. Curr Opin Psychiatry. 2017;30(6):423-437.
Comments
Post a Comment