Mapping gut parasitism patterns in a cohort of Egyptians | Scientific ... - Nature.com
Abstract
In developing countries, the prevalence of intestinal parasitic infection is still significant, particularly due to geographical and socioeconomic variables. The objective of this study was to map the distribution pattern of intestinal parasitic infection in a cohort of the Egyptian population, as well as to assess associated risk factors. A cross-sectional hospital-based study was conducted on 386 patients. A single fecal specimen was collected from the study individual and examined microscopically for the detection of parasitic infection. DNA was extracted from all samples and utilized to amplify Entamoeba histolytica complex species, Cryptosporidium species, Giardia intestinalis assemblages, and Blastocystis species using PCRs. Typing of Cryptosporidium species and Giardia intestinalis assemblages was performed using restriction enzymes RasI and HaeIII respectively. While Blastocystis spp. subtypes (ST) were identified through sequencing of PCR products and phylogenetic analysis. 59.6% (230/386) of the study patients were infected with one or more intestinal parasites, 87.4%; 201/230 of patients had mono-parasitic infections, and 12.6%; 29/230 had multiple-parasitic infections (P < 0.0001). The predominant protozoa were Blastocystis, followed by Entamoeba histolytica complex, and Giardia intestinalis both as mono-parasites and as part of multiple parasites. Molecular assays showed that Blastocystis ST3, Entamoeba dispar, Giardia intestinalis assemblage B, and Cryptosporidium hominis were the most prevalent species. Intestinal parasitic infection was significantly associated with age, gender, residence, and water source. Multi-parasitism showed that residency in a rural area was a risk factor (OR 4.49; 95% CI 1.51–13.37; P = 0.007). Egyptians residing in rural areas have a high prevalence of intestinal multi-parasitism. Therefore, to lessen the prevalence and effects of these infections in this group, effective and sustainable control methods, providing health education focusing on good personal hygiene habits, and providing a safe drinking water supply should be implemented.
Introduction
Intestinal parasites (IPs) are widespread throughout the world and have a significant negative influence on morbidity and mortality, particularly in developing countries1,2. IPs have been linked to stunting, physical weakness, and poor academic performance in children. By interacting with absorptive surfaces, physically obstructing the intestinal lumen, producing proteolytic chemicals, and consuming nutrients destined for the body, IPs reduce nutrient intake in the body. Due to their heightened susceptibility to nutritional inadequacies, children are more vulnerable to the effects of intestinal parasitic infections3,4. Furthermore, IPs-related disorders display a heavy burden. Over two billion people are affected globally by IPs, of which 300 million have severe morbidity and approximately 4.5 billion people are at risk. The World Health Organization reported that there were 200 million instances of Giardia lamblia, 800 million cases of Ascaris lumbricoides, 700 million cases of hookworm, 500 million cases of Trichuris trichuria, and 500 million cases of Entamoeba histolytica/ dispar worldwide. According to earlier estimates, IPs result in an annual loss of 39 million disability-adjusted life years, resulting in serious health and financial problems. However, the biggest problem of IPIs is that 90% of infected people are asymptomtic5,6.
The main intestinal protozoans that infect humans are Entamoeba histolytica, Balantidium coli, Giardia lamblia, Isospora belli, and Cryptosporidium species7. Other species, like Blastocystis sp. and Dientamoeba fragilis, are disputed pathogens, their presence is not associated with clinical significance and their role in people who have digestive symptoms is currently debatable. However, few clinics and laboratories routinely test for Dientamoeba fragilis and Blastocystis sp.8. Similarly, many other non-pathogenic intestinal protozoa can be found in humans that are not associated with diseases, including Entamoeba coli, Entamoeba dispar, Entamoeba hartmanni, Entamoeba polecki, Endolimax nana, Iodamoeba bütschlii, and Chilomastix mesnili9. Intestinal helminths including Ascaris lumbricoides (A. lumbricoides), Trichuris trichiura (T. trichiura), and hookworm species (Necator americanus and Ancylostoma duodenale) are grouped under soil-transmitted helminths, which are highly prevalent in developing countries10. In Egypt, intestinal schistosomiasis (S. mansoni) is prevalent in the Nile Delta while urogenital schistosomiasis (S. haematobium) in the Nile valley south of Cairo, down to Aswan and beyond. Epidemiological studies have shown that in endemic areas, multiparasitism is more frequent than single infections11,12,13. Geographical, behavioral, biological, and socioeconomic factors all influence how prevalent these illnesses are. IPs are directly related to the hot and humid climate of the tropics, the lack of access to clean water, the unsanitary environmental conditions, overcrowding, and low family income. These circumstances facilitate intestinal parasite growth, transmission, and exposure14.
The majority of research on co-infections with several parasites, which occurs when infectious agents coexist in the same host and can have a prevalence of up to 80% in some populations, has focused on humans15. These co-infections may result from a variety of environmental factors, such as contagious settings and transmission paths, and may be aided or hindered by direct or indirect interactions between different parasite species16. The interaction between different parasite populations (within and between hosts) and host populations, rather than associations play a significant role17. Though the specifics of these interactions within the host are unknown, some are sought to be synergistic where the presence of one parasite may encourage the occurrence of future parasitic infections, while others are thought to be antagonistic where parasites compete for the same ecological niche within the host18.
Studies carried out in several governorates over the past few years to determine the prevalence of IPs and the risk factors associated with them among the Egyptian population have found that IPs continue to be a problem for public health. Therefore, for adequate planning and execution of efficient preventative and control strategies, frequent assessment of IPs prevalence and identification of the related risk factors is required. Therefore, the current study's objective was to investigate the prevalence of multiparasitism and intestinal parasites. Additionally, to study the relationships between multiple parasite infections and their risk factors in comparison to single parasite infections or complete lack of infection in the Egyptian population.
Results
The diagnostic yield of microscopy and molecular assays to document the presence of intestinal parasites in patients' fecal samples were shown in Table 1 and Supplementary figure.
Intestinal parasites were microscopically detected in the stool specimens of 230 patients among the examined 386 Egyptian patients with a prevalence rate of 59.6%. Blastocystis species was the predominant intestinal parasite, both as a mono-parasites (110/230 [47.8%]) or part of a multi-parasites (24/230 [10.4%]). Single intestinal parasites were detected in 87.4% (201/230) of the microscopically examined stool specimens. There was a clear predominance of intestinal protozoa (225/230 [97.8%]) compared to intestinal helminths (5/230 [2.2%]). Blastocystis was the predominant protozoa (47.8%), followed by Entamoeba histolytica complex (26%), and Giardia intestinalis (10.4%). Multiparasitism was detected in 12.6% (29/230) of the patients, 27 (11.8%) of them had two parasites and 2 (0.8%) of them had three parasites.
The prevalence of parasites was confirmed by PCR, Blastocystis copro-DNA was detected in 139 (60.4%), of which 134 (58.2%) were positive by microscopy, no samples were positive by microscopy, and negative by PCR. The diagnostic performance of Blastocystis showed that the sensitivity of microscopy was 96.40% compared to PCR results.
On the other hand, 27(11.7%) and 68(29.6%) of the examined specimens were molecularly positive for Giardia intestinalis and Entamoeba histolytica complex, respectively while, 31 (11.9) and 76 (33%) were positive microscopically (Table 2). The diagnostic performance of Giardia intestinalis and Entamoeba histolytica complex microscopy in diagnosis displayed a sensitivity of 100% in comparison with PCR which showed a sensitivity of 87.10%, and 89.47% respectively.
Cryptosporidium species were in three stool specimens by both microscopy and nested PCR with the same sensitivity, all of which were Cryptosporidium hominis. Giardia intestinalis assemblages A and B were detected, assemblage B was the predominant assemblage (21/27 [77.8%]).
Entamoeba histolytica complex species were molecularly identified using multiplex PCR in 68 patient samples. Entamoeba histolytica (20.6%; 14/68) was detected in one-fifth of the molecularly positive samples (Table 3). Regarding the nonpathogenic species, Entamoeba dispar was the most common species (44.1%; 30/68), followed by Entamoeba moshkovskii (35.3%; 24/68).
Only ten PCR products positive for Blastocystis showed high-quality sequences, among them three STs were detected (ST1, 2, and 3). The three detected STs displayed more or less equal distribution with ST3 being the most prevalent ST among the sequenced samples (4/10; 40%) followed by ST1 and ST2 (30% (3/10) each).
All obtained sequences were deposited in the GenBank database with accession numbers (OR015950–OR015959) (Fig. 1).
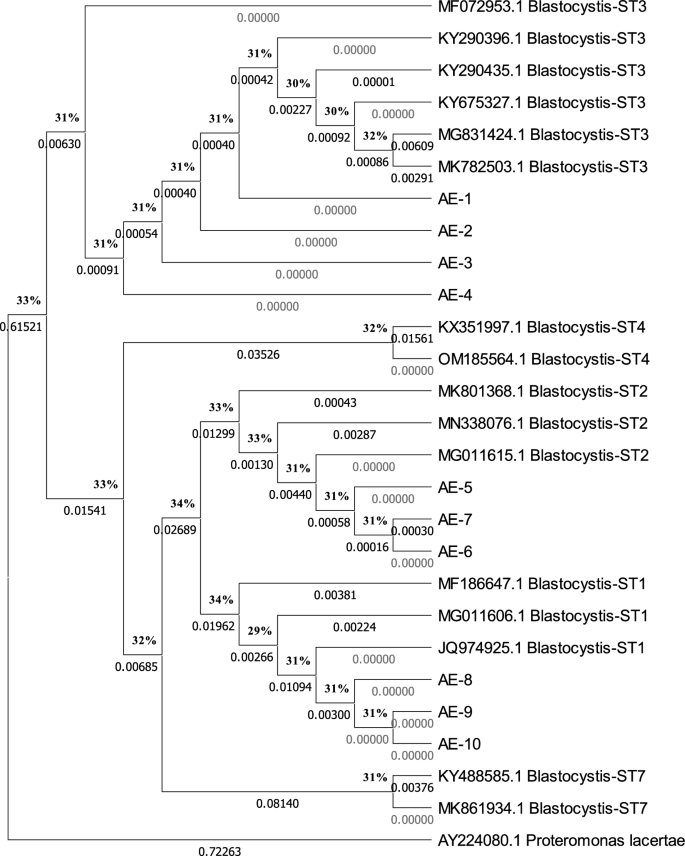
Dendrogram representing the neighbor-joining phylogenetic tree of the three Blastocystis subtypes (start with the abbreviation AE followed by the sample number) from our study patients compared to reference subtypes from the GenBank (the accession number is written before their names and subtypes). The bootstrap analysis is based on 1000 replicates.
The age of the study individuals ranged from 3 months to 75 years with a mean and standard deviation of 29.17 ± 18.83. Most of the infected participants were male (59.1%), rural residents (61.7%), and consuming tap water (70%). There were statistically significant differences between infected and non-infected participants regarding age, gender, residence, and water source (Tables 4, 5, 6). The most-reported GIT symptoms among infected participants were abdominal pain (51.3%), and diarrhea (37.8%), with highly significant differences between infected and non-infected participants (Tables 4, 5, 6).
The association between infection with one parasite or more than one parasite (multiparasitism) and the individuals' sociodemographic and clinical data was studied (Table 7). Participants with poly-parasites had higher odds of reporting sociodemographic data such as residence in a rural area and animal contact compared to participants with mono-parasitic infection (P < 0.05). There was a trend for a higher likelihood of abdominal pain and diarrhea among individuals with poly-parasitic infection than mono-parasitic infection (P < 0.05). No association was found between polyparasitic infection and (age, gender, water source, vomiting, and fever) (P > 0.05).
Discussion
This study determined the prevalence of intestinal parasitic infection among a cohort of Egyptians, in addition to investigating mono- and poly-parasitic patterns with their associated risk factors. Epidemiological studies are essential for determining the prevalence of intestinal parasitic infections, identifying risk factors, and creating effective prevention and control strategies, all of which continue to be a major health concern in developing countries such as Egypt19.
There was a relatively high prevalence of intestinal parasites (59.6%) in the studied cohort of Egyptians which was similar to a study by Omar and Abdelal20, who reported a 56% prevalence of intestinal parasitic infection among Egyptian patients. Ahmed and Abu-Sheishaa19 reported that IPs represented an overall prevalence of 32.9% among school children. This variation in findings may be due to differences in sociodemographic and environmental factors with different exposures to risk factors.
Of the infected individuals, 201 (87.4%) had mono-parasite, 29 (12.6%) had multiple-parasites with double infection (27, 11.8%), and triple infection (2, 0.8%), which can be explained by sharing the same social-ecological contexts that encourage the occurrence and transmission of these parasitic diseases. In terms of the detected intestinal parasites, Blastocystis was the predominant parasite, for both a mono-infection (110, 48.7%) and coinfection (24, 10.4%), followed by Entamoeba histolytica complex (26%), and Giardia intestinalis (10.4%). This finding is consistent with a study conducted by Diarthini in Karangasem (Bali, Indonesia), where Blastocystis spp. was shown to be the most common parasite among primary school students21. In poly-parasitic infections, Blastocystis spp. was the most common protozoa. This finding was consistent with a study by Diarthini et al.21 that identified Blastocystis spp. to be frequently present in poly-parasitic infections with Giardia intestinalis, Entamoeba histolytica complex, and Entamoeba coli. In contrast, previous studies conducted in Egypt reported Giardia intestinalis as the most prevalent parasitic infection22,23.
In this study, molecular methods for identifying human infections and protozoa were standardized and evaluated. The minimum amount of DNA per µL or per PCR reaction was used to determine the sensitivity of all standardized molecular techniques (PCR, nested or semi-nested PCR, PCR–RFLP). Where sensitivity is the smallest number of living forms that can be detected by molecular assays. Standardized tests made it possible to identify species of the same genus that were not distinguishable by microscopic examination, as in the case of the differentiation between E. histolytica, E. dispar, and E. moshkovskii, as well as to identify genotypes (Blastocystis spp.) or assemblages (G. intestinalis) that were crucial for using molecular epidemiology or transition studies.
Depending on the method chosen for parasite identification, prevalence data can readily be changed, either positively or negatively. Laboratory diagnosis of Blastocystis can be fairly difficult. Despite being the preferred method for diagnosing Blastocystis all around the world, direct microscopic examinations have limited applications in clinical microbiology labs and epidemiological studies. Polymorphic creatures and inanimate objects at wet mounts may be mistaken for other living things. When compared to PCR, our investigation showed that direct wet mount had a less sensitivity (96.4%). The three detected Blastocystis STs displayed more or less equal distribution with ST3 being the most prevalent ST among the sequenced samples. This result agrees with Ahmed et al.20 who reported three Blastocystis STs (ST1, ST2, and ST3), with ST3 (45.5%) representing the most common subtype. DNA sequencing and phylogenetic analysis of Egyptian Blastocystis isolates identified three different subtypes. Further studies are required to determine the distribution of STs in the general population. Nonetheless, our study is a contribution to the understanding of the molecular epidemiology, transmission patterns, and genetic diversity of Blastocystis.
With the use of Lugol, the cysts of Entamoeba spp. can be identified using light microscopy based on their morphological traits24. Cysts of the pathogenic amoeba E. histolytica resemble the non-pathogenic amoebae E. moshkovskii and E. dispar in terms of morphology. Other molecular epidemiology studies have identified E. moshkovskii as the causative agent of gastrointestinal symptoms using multiplex PCR and the detection of ribosomal SSU identical to 16S25. Our investigation showed that PCR had (89.47%) less sensitivity. In this study, concerning Entamoeba histolytica complex, our findings demonstrated that most samples were attributed to Entamoeba dispar and Entamoeba moshkovskii. This result is in line with previous studies carried out in Egypt by El-Badry et al.26, and in Iran, by Fallah et al.27 who reported Entamoeba dispar as the most prevalent Entamoeba species. In contrast, a study conducted in the United Arab Emirates found Entamoeba histolytica to be more prevalent28. In the present study, there were four cases of co-infections, with the three different Entamoebae species.
In this study, G. intestinalis was identified from fecal samples using morphological and molecular detection methods. Giardia diagnosis in medical labs is based on wet mount preparation of patient feces and ocular detection by light microscopy. These procedures must be carried out by qualified microscopists and medical laboratory technicians. On the other hand, these methods may not be sensitive enough to find small quantities of expelled Giardia cysts in fecal samples and are unable to distinguish between the genetic assemblages of G. intestinalis isolates. To find G. intestinalis cysts in feces, molecular detection methods based on PCR have been developed. Our investigation showed that PCR had (87.1%) less sensitivity. G. intestinalis cysts can be genotyped using these molecular techniques. Genotyping analysis for Giardia intestinalis showed assemblage B predominance (77.8%), this result is similar to previous studies in Egypt that reported the predominance of assemblage B29,30,31. Genotyping for Cryptosporidium revealed only cryptosporidium hominin.
Regarding age, gender, residence, and water source, there was a statistically significant difference between infected and non-infected individuals. These study findings are similar to previous studies which revealed significant differences regarding age32,33,34, gender differences33,35; which can be explained by considerable outdoor activity and increased exposure to infectious diseases, and in rural areas36,37, this can be explained by their risky behavior, such as interaction with domestic animals, poor hygiene, defecating in an open field of agriculture near water sources, all of which increase the level of parasite contamination in the soil38. Also, there were highly significant differences between the infected and non-infected individuals regarding the GIT symptoms (abdominal pain and diarrhea) (P < 0.0001). These findings agree with the findings of similar studies39. As expected, we observed a significantly higher multiparasitism infection rate among participants with gastrointestinal symptoms compared to the asymptomatic group.
In the current study, polyparasitism was found to be more common among males than females, but this difference was not statistically significant. In contrast, a study from Nigeria revealed that females are more vulnerable to polyparasitism than males35. The variation seems to support the idea that male outdoor activities may increase relative interaction with the parasitic infectious stages. Our findings showed the risk for polyparasitism significantly increased with residency in rural communities. This finding is in agreement with reports from other parts of Africa, especially the rural communities40,41. Moreover, animal contact showed a highly significant association with polyparasitism among our study individuals. This could be attributed to the zoonotic nature of the parasitic infection which is still unresolved in literature. Also, there was a significant association between polyparasitism and both abdominal pain (P = 0.018) and diarrhea (P < 0.0001). These findings agreed with Suwarna Pawar et al.42 who reported that multiple parasitic infestations in low socioeconomic populations can be a cause of diarrhea.
In the current study, a major strength was the inclusion of a wide spectrum of age groups, as this facilitates the comparison of infection prevalence and their association with age. On a broader scale, the identification of individuals with polyparasitism using molecular tools, such as PCR, is important as it can provide a measure of disease burden and also serve as a guide for the development of specific prevention and control interventions against multiple parasites. Our results contribute toward mapping the molecular epidemiology, transmission patterns, and genetic diversity of parasitic infections at a regional and global scale.
Our study was limited by being a single center institutional study including patients attending TBRI which could be the reason that there were relatively few worm infections and many protozoans, and very few Cryptosporidium. Another limitation is the lack of data concerning certain risk factors, including socioeconomic status, educational level of patients, and family history of intestinal symptoms that would help in the detection of prevalence-associated risk factors.
Conclusion
Based on our study findings, the studied cohort of Egyptians had a relatively high rate of intestinal parasitism. The most prevalent parasites were Blastocystis, followed by Entamoeba histolytica complex, and Giardia intestinalis. Age, gender, residing in a rural area, and water source were all potential risk factors for intestinal parasitism. Additionally, there was a significantly substantial correlation between GIT symptoms and parasite infection. One-eighth of our research population, particularly in rural Egypt, had multiple intestinal parasitic infections. Understanding the distribution pattern of intestinal parasites would help thus in the strategic planning of prevention and control measures.
Methods
Study design and population
A cross-sectional study was conducted from April 2020 to May 2021. A single stool specimen was collected from 386 Egyptian, aged from 3 months to 75 years, attending Theodor Bilharz Research Institute (TBRI) clinics, having gastrointestinal symptoms, or as part of a routine check-up. A questionnaire was used to collect relevant sociodemographic and clinical data. Participants taking antiparasitic treatment within the last 2 months were excluded from the study.
Sample size determination and sampling technique
Using the general formula, n = z2p (1 − p)/d2, the sample size was calculated with a 95% confidence level, a 5% margin of error, and a 21% response distribution. The calculated sample size was 285 samples43. The used sample size was 314 people accounting for a 10% non-response rate.
Copro-parasitological examination
All collected stool specimens were examined microscopically using both saline solution and Lugol temporary stain, before and after using the formalin-ethyl acetate concentration method44 to detect fecal parasitic stages. Feces were smeared and stained by a modified acid-fast (AF) stain for the detection of Cryptosporidium and other coccidian oocysts45.
Molecular assays
Extraction of genomic DNA
After the initial thermal shock (10 cycles of freezing in liquid nitrogen and thawing at 95 °C) of fecal specimens, DNA extraction was performed using the DNA Stool Mini Kit (QIAGEN, Hilden, Germany), according to the instructions of the kit.
PCR assays
Extracted copro-DNA were amplified using three PCRs, (1) multiplex PCR (m-PCR) to detect the three Entamoeba histolytica complex species; Entamoeba histolytica, Entamoeba dispar and Entamoeba histolytica Entamoeba moshkovskii (2) two nested PCR to detect Cryptosporidium species and Giardia intestinalis, and (3) conventional PCR to detect Blastocystis species. The used primer sequences and PCR reaction conditions of the used PCRs were listed in Table 8. The PCR products were visualized on 1.5% agarose gel and stained with ethidium bromide under a UV light system.
Nested PCR-Restriction Fragment Length Polymorphism (RFLP).
Cryptosporidium genotypes and Giardia intestinalis assemblages were detected by the banding patterns in the restriction analysis of nested PCR products of Cryptosporidium species and Giardia intestinalis with restriction enzymes RasI and HaeIII, respectively. Digestion products were fractionated on 3% Metaphor agarose after ethidium bromide staining.
Sequencing and phylogenetic studies of Blastocystis spp
Thermo Scientific Gene JET PCR Purification Kit was used to purify the positive PCR products for Blastocystis, and sequencing was done using the primer pair RD5 and BhRDr, and Big-Dye® Terminator v3.1. Ready Reaction Cycle Sequencing Kit (Applied Biosystems, Foster City, CA, USA) was also used following the manufacturer's instructions for the ABI Prism 310 genetic analysis. Sequences from Blastocystis isolates were corresponded with reference sequences in the GenBank database using online BLAST software at the National Center for Biotechnology Information (NCBI) (http://www.ncbi.nlm.nih.gov/BLAST). All sequences were aligned using the BioEdit software's ClustalW tool50. The phylogenetic tree for the sequences was made using the neighbor-joining approach51 with the Molecular and Evolution Genetic Analysis X (MEGA10) program52. Bootstrapping was used to assess the trustworthiness of the phylogenetic tree (1000 replicates). The Maximum-Likelihood approach with the Tamura-3 parameter substitution model was used with MEGA10 to calculate the evolutionary distances.
Statistical analysis
For descriptive data, the data are displayed as numbers and percentages. For categorical data, the chi-square and Fisher's exact tests were utilized to evaluate differences. The odds ratio and 95% confidence interval for each factor that affected the prevalence of intestinal parasite infection in the population under study were calculated using univariate analysis. The cutoff for significance was P < 0.05. The statistical program for social science (SPSS) Version 28 for Windows was used for all statistical analyses (SPSS Inc., Chicago, IL, USA).
Ethical considerations
This study was performed after approval of the Research Ethical Committee of Theodor Bilharz Research Institute (TBRI-REC), with the serial number of protocol: PT (499). The TBRI-REC is registered at the Office for Human Research Protections, US Department of Health and Human Services, and operates under Federal Wide Assurance No. FWA00010609. All the approved research work complies with the World Medical Association Codes of Ethics (Declaration of Helsinki) for experiments with humans. Participant informed consent was obtained from all participants and/or their legal guardians.
Data availability
All data generated or analyzed during this study are included in this published article.
References
Al-Yousofi, A. et al. Prevalence of intestinal parasites among immunocompromised patients, children, and adults in Sana'a, Yemen. J. Trop. Med. 2022, 5976640. https://doi.org/10.1155/2022/5976640 (2022).
Ifeoma, A., Teke, A., Aviwe, B., Oladimeji, O. & Abaver, D. Prevalence of intestinal parasites in HIV/AIDS-infected patients attending clinics in selected areas of the Eastern Cape. Microbiol. Res. 13, 574–583. https://doi.org/10.3390/microbiolres13030040 (2022).
Opara, K. N. et al. The impact of intestinal parasitic infections on the nutritional status of rural and urban school-aged children in Nigeria. Int. J. MCH AIDS 1(1), 73–82 (2012).
Ihejirika, O. C., Nwaorgu, O. C., Ebirim, C. I. & Nwokeji, C. M. Effects of intestinal parasitic infections on nutritional status of primary children in Imo State Nigeria. Pan Afr. Med. J. 33, 34. https://doi.org/10.11604/pamj.2019.33.34.17099 (2019).
Shrestha, A. et al. Intestinal parasite infections and associated risk factors among schoolchildren in Dolakha and Ramechhap districts Nepal: A cross-sectional study. Parasites Vectors 11, 532 (2018).
World Health Organisation Soil-Transmitted Helminth infections 2020. Available from: https://www.who.int/news-room/fact-sheets/detail/soil-transmitted-helminth-infections. Accessed 15 Aug 2021 (2020).
Hemphill, A., Müller, N. & Müller, J. Comparative pathobiology of the intestinal protozoan parasites Giardia lamblia, Entamoeba histolytica, and Cryptosporidium parvum. Pathogens 8(3), 116. https://doi.org/10.3390/pathogens8030116 (2019).
Sarzhanov, F. et al. Investigation of neglected protists Blastocystis sp. and Dientamoeba fragilis in immunocompetent and immunodeficient diarrheal patients using both conventional and molecular methods. PLoS Negl. Trop. Dis. 15(10), e0009779. https://doi.org/10.1371/journal.pntd.0009779 (2021).
Issa, R. Non-pathogenic protozoa (review article). Int. J. Pharm. Pharm. Sci. 6, 30–40 (2014).
Goshu, A., Alemu, G. & Ayehu, A. Prevalence and intensity of soil-transmitted helminths and associated factors among adolescents and adults in Bibugn Woreda, Northwest Ethiopia: A community-based cross-sectional study. J. Trop. Med. 2021, 7043881. https://doi.org/10.1155/2021/7043881 (2021).
Al-Delaimy, A. K. et al. Epidemiology of intestinal polyparasitism among Orang Asli school children in rural Malaysia. PLoS Negl. Trop. Dis. 8(8), e3074. https://doi.org/10.1371/journal.pntd.0003074 (2014).
Llewellyn, S. et al. Application of a multiplex quantitative PCR to assess prevalence and intensity of intestinal parasite infections in a controlled clinical trial. PLoS Negl. Trop. Dis. 10(1), e0004380 (2016).
Donohue, R. E., Cross, Z. K. & Michael, E. The extent, nature, and pathogenic consequences of helminth polyparasitism in humans: A meta-analysis. PLoS Negl. Trop. Dis. 13(6), e0007455 (2019).
Elmonir, W. et al. Prevalence of intestinal parasitic infections and their associated risk factors among preschool and school children in Egypt. PLoS One 16(9), e0258037. https://doi.org/10.1371/journal.pone.0258037 (2021).
Hoarau, A. O. G., Mavingui, P. & Lebarbenchon, C. Coinfections in wildlife: Focus on a neglected aspect of infectious disease epidemiology. PLoS Pathogens 16(9), e1008790 (2020).
Vaumourin, E., Vourc'h, G. & Gasqui, P. The importance of multiparasitism: Examining the consequences of co-infections for human and animal health. Parasites Vector 8(1), 545 (2015).
Wood, C. L. et al. Parasites alter community structure. Proc. Natl. Acad. Sci. U. S. A. 104(22), 9335–9339. https://doi.org/10.1073/pnas.0700062104 (2007).
Kajero, O. T. et al. Co-infection of intestinal helminths in humans and animals in the Philippines. Trans. R. Soc. Trop. Med. Hyg. 116(8), 727–735. https://doi.org/10.1093/trstmh/trac002 (2022).
Ahmed, H. M. & Abu-Sheishaa, G. A. Intestinal parasitic infection among school children in Dakahlia governorate, Egypt: A cross-sectional study. Egypt. Pediatr. Assoc. Gaz 70, 6. https://doi.org/10.1186/s43054-021-00093-9 (2022).
Omar, M. & Abdelal, H. O. Current status of intestinal parasitosis among patients attending teaching hospitals in Zagazig district, Northeastern Egypt. Parasitol. Res. 121, 1651–1662. https://doi.org/10.1007/s00436-022-07500-z (2022).
Diarthini, N. L. P. E. et al. Blastocystis and other intestinal parasites infections in elementary school children in Dukuh Village, Karangasem District, Bali. Indones. J. Trop. Infect. Dis 7, 57–61 (2018).
Mohamed, A. M. A., Bayoumy, A. M., Abo-Hashim, A. H., Ibrahim, A. A. & El-Badry, A. A. Giardiasis in symptomatic children from Sharkia, Egypt: Genetic assemblages and associated risk factors. J. Parasit. Dis. 44(4), 719–724. https://doi.org/10.1007/s12639-020-01254-0 (2020).
Morsy, S. M., Elmatrawy, O. M., Rubio, J. M., El-Badry, A. A. & Hassan, M. A. Enteric pathogenic protozoa from misdiagnosis to overmedication in Egypt: A need for molecular diagnosis. Comp. Clin. Pathol. 31, 765–772 (2022).
Comments
Post a Comment