Effect of experimental hookworm infection on insulin resistance in people at risk of type 2 diabetes - Nature.com
Abstract
The reduced prevalence of insulin resistance and type 2 diabetes in countries with endemic parasitic worm infections suggests a protective role for worms against metabolic disorders, however clinical evidence has been non-existent. This 2-year randomised, double-blinded clinical trial in Australia of hookworm infection in 40 male and female adults at risk of type 2 diabetes assessed the safety and potential metabolic benefits of treatment with either 20 (n = 14) or 40 (n = 13) Necator americanus larvae (L3) or Placebo (n = 13) (Registration ACTRN12617000818336). Primary outcome was safety defined by adverse events and completion rate. Homoeostatic model assessment of insulin resistance, fasting blood glucose and body mass were key secondary outcomes. Adverse events were more frequent in hookworm-treated participants, where 44% experienced expected gastrointestinal symptoms, but completion rates were comparable to Placebo. Fasting glucose and insulin resistance were lowered in both hookworm-treated groups at 1 year, and body mass was reduced after L3-20 treatment at 2 years. This study suggests hookworm infection is safe in people at risk of type 2 diabetes and associated with improved insulin resistance, warranting further exploration of the benefits of hookworms on metabolic health.
Similar content being viewed by others

Ultra-processed foods and food additives in gut health and disease

Two-year effects of semaglutide in adults with overweight or obesity: the STEP 5 trial

Microbiota in health and diseases
Introduction
Metabolic syndrome (MetS) represents a collection of related metabolic conditions, including dysregulated lipid homoeostasis, hypertension, insulin resistance, and abdominal obesity, that increase the likelihood of developing chronic diseases such as type 2 diabetes mellitus (T2D) and cardiovascular disease1. T2D is a complex illness associated with hyperglycaemia and insulin resistance, where long-term and costly medical care is usually required to prevent complications. The prevalence of T2D is increasing globally, with more than half a billion adults already diagnosed2; hence there is a pressing need to develop new preventative approaches to limit the burden of T2D on individuals and health systems.
The soaring global prevalence of T2D is undoubtedly related to lifestyle factors such as an energy-dense diet and a sedentary lifestyle. In this context, the detrimental role of systemic, low-grade inflammation in promoting insulin resistance is well-established3. In lean adipose tissue, there exists an anti-inflammatory environment, including regulatory T cells, eosinophils, and alternatively activated macrophages that are stimulated by type 2 cytokines such as interleukin (IL)−4, IL-5, and IL-13. Conversely, in obesity there is a pro-inflammatory milieu involving type 1 cytokines such as IFNγ and TNF, classically-activated macrophages4, and a dysregulated gut microbiome5. This biased Type-1 immune response aggravates insulin resistance through stress-activated kinases that target intermediates in the insulin-signalling pathway6. It follows that maintaining the systemic and adipose-specific inflammatory balance in favour of type 2 or regulatory immune response is a rational approach to limiting the inflammatory cascade and preventing the ensuing insulin resistance seen in metabolic disease.
Parasitic helminths (worms) co-evolved with humans and remain endemic in regions of the world with less metabolic and inflammatory diseases7,8,9,10. Helminth infections are associated with type 2 immune responses such as eosinophilia, elevated IL-4, −5, and −13, Type-2 innate lymphoid cell responses, and modulation of the gut microbiome11. Emerging evidence supports the hypothesis that eradicating worms from industrialised regions may have partly contributed to the increased prevalence of immune-mediated diseases such as T2D8,12. For example, human epidemiological studies suggest that the presence of helminth infections is associated with lessened inflammatory responses and improved glucose homoeostasis10,12,13, and two systematic reviews and meta-analyses concluded that adults with previous or current worm infection typically enjoy improved metabolic function14,15. While cross-sectional studies support the idea of a protective role for worms in metabolic disease, they did not establish causality.
Recent deworming studies provided some causative evidence. The removal of worms from previously-infected individuals was associated with increased insulin resistance (elevated homoeostatic model assessment for insulin resistance, HOMA-IR)16, elevated serum insulin and glucagon17, enhanced hyperglycaemia and risk of metabolic disease18, and worsened blood lipid profiles19. Experimental mouse studies corroborate findings from human studies, where infection with various worm species caused improvements in metabolic indices, type 2 immune responses, and alterations to the gut microbiome20,21,22,23,24. However, to date, there have been no studies in humans testing whether a controlled helminth infection is safe, can improve metabolic health, and potentially prevent progression to T2D.
Previously, we and others have established the safety of infecting human volunteers with low doses of hookworms in various inflammatory diseases25,26,27. While none of these studies investigated metabolic health outcomes, it is well reported that hookworms elicit type 2 and regulatory immune responses26 and changes in the microbiome28 that may be beneficial in the context of T2D. The primary aim of this randomised, double-blinded, placebo-controlled Phase 1b clinical trial was to establish the safety, tolerability, and potential metabolic benefits of experimental infection with infective third-stage larvae (L3) of the human hookworm Necator americanus in otherwise healthy adults with metabolic syndrome and at risk of developing T2D. Based on previous animal and deworming studies, we hypothesised that hookworm infection would be safe and improve the key metabolic outcome for the study, HOMA-IR, which assesses longitudinal changes in insulin sensitivity that correlate well with estimates derived via the euglycaemic clamp29. In this study we demonstrate that hookworm infection is safe and well-tolerated in people at risk of type 2 diabetes, and provide proof of principle that hookworm treatment may stabilise or improve key determinants of metabolic health such as insulin resistance.
Results
Study population
We conducted a 2-year Phase Ib randomised, double-blinded, three-arm placebo-controlled trial of experimental hookworm infection (either 20 or 40 infective third-stage larvae, L3) in otherwise healthy people at risk of T2D (Fig. 1A). Recruiting progressed between January 2018 and June 2020, with 85 potential participants meeting screening criteria, of which 41 met the inclusion/exclusion criteria to proceed to randomisation (4 short of the recruitment target). Forty-four participants were excluded due to not having elevated baseline HOMA-IR (n = 27), not responding to communication (n = 11) or excluded medications or medical conditions (n = 6) (Fig. 1B). One participant who qualified for the study dropped out prior to their baseline visit. Forty participants were randomised and constituted the intention-to-treat (ITT) population (Table 1). Thirteen participants were allocated to receive Placebo treatment, 14 to receive a dose of 20 hookworm larvae (L3-20) and 13 to receive a dose of 40 hookworm larvae (L3-40). (Fig. 1B). The majority of participants (85%) were of Caucasian descent. Baseline age and HOMA-IR were higher in the L3-20 group. One participant who was randomised into the Placebo group unintentionally received an L3-20 treatment due to a labelling error. This participant was included in the Placebo group for the ITT analysis but in the L3-20 group for per-protocol analyses.
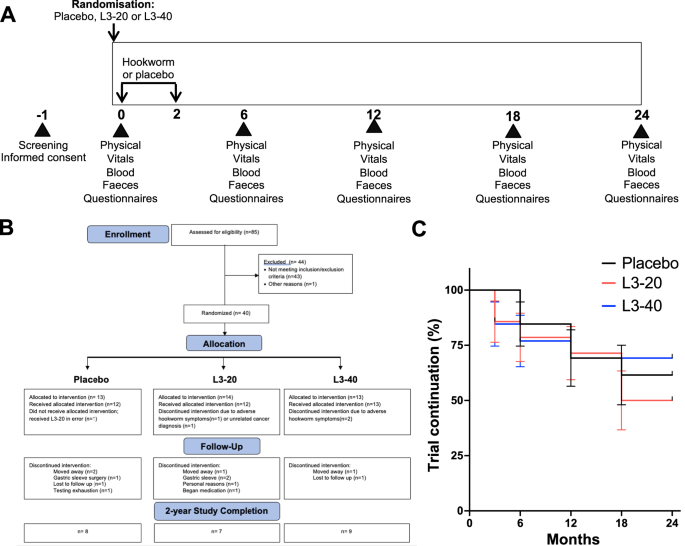
A After screening and informed consent, participants were allocated to receive either placebo (chilli pepper solution) or a total of 20 (L3-20) or 40 (L3-40) N. americanus hookworm larvae delivered to the skin over 2 occasions, at month 0 and month 2. Participants underwent evaluation visits every 6 months, where physical and vitals exams were undertaken, adverse events were reviewed, and biological samples and questionnaires were collected for analysis of safety, pathology, well-being, diet and exercise habits. B CONSORT chart showing flow of patients through the clinical trial, and reasons for early termination. C Kaplan–Meier analysis of rates of trial continuation (percentage survival and standard error of the mean) in each group during the 2-year study (Placebo n = 13, L3-20 n = 14, L3-40 n = 13; Log-rank test for trend, p = 0.832). Source data are provided as a Source Data File.
Adverse events (AEs)
The study's primary outcome was the safety and tolerability of hookworm treatment, assessed by an intention to treat analysis of the frequency and severity of AEs. A total of 20 AEs and no serious AEs were reported (Table 2). As expected, gastrointestinal (GI) adverse events occurred in the L3-20 and L3-40 treatment groups (Table 2), consistent with the worms arriving in the gut and attaching to the intestinal wall. These AEs were experienced by 44% of hookworm-treated participants and included bloating, nausea, vomiting, constipation, diarrhoea, epigastric upset, hungry feeling, stomach cramps and abdominal pain, which were typically mild-moderate and resolved without medical intervention. One GI-related symptom (5%) was recorded as severe, and three warranted early removal of the participants from the study (1 in the L3-20 group, 2 in the L3-40 group) and provision of deworming medication. Two of these individuals recovered promptly after deworming, while symptoms in one participant persisted, indicating their symptoms may have been unrelated to hookworm. No GI-related AEs occurred in the Placebo group. No participant developed anaemia (Supplementary Fig. 1), the primary clinical effect of moderate to heavy hookworm infection. AEs deemed unrelated to worm infection were reported across all groups and included one case each of concussion, laryngitis, appendicectomy, gynaecological procedure, salmonella infection acquired overseas, breast cancer diagnosis, erythema, and dermatitis. The chi-square test for trend revealed a significant linear trend for AEs, χ2 (1, N = 40) = 3.846, p = 0.049, with more AEs occurring in the hookworm treatment groups compared to the Placebo group, as anticipated based on studies in other patient populations30.
Study Progression and well-being
Rates of trial completion and participant mood and well-being were safety outcomes, which were all conducted using per protocol analyses. The CONSORT Flow Diagram (Fig. 1B) and Kaplan–Meier curve (Fig. 1C) detail study progression. Early dropouts (0-6 months) included the 3 participants with GI symptoms and one participant in the L3-20 group that was removed from the study at 3 months due to an unrelated cancer diagnosis (Fig. 1B). Reasons for early terminations later in the study included 4 participants moving away (Placebo n = 2, L3-20 n = 1, L3-40 n = 1), 1 for undisclosed personal reasons (L3-20), 3 for failure to respond to communication or testing exhaustion (Placebo n = 2, L3-40 n = 1), and 4 for starting medication (L3-20, n = 1) or undergoing gastric sleeve surgery (Placebo n = 1, L3-20 n = 2) that could interfere with the trial outcomes. Four participants (Placebo n = 1, L3-20 n = 2, L3-40 n = 1) missed one evaluation visit each but completed the remaining evaluation visits. Twenty-four of the 40 randomised participants completed the trial, including 8 (62%) in the Placebo, 7 in the L3-20 (50%) and 9 in the L3-40 group (69%). The difference in study completion between groups was not significant (Fig. 1C, Log-rank test for trend, p = 0.832). Monitoring of participant mood and depressive state via the Patient Health Questionnaire-9 (PHQ-9) revealed that median scores in the Placebo group remained relatively stable throughout (Table 3). There was a trend for reduced median PHQ-9 scores (suggestive of improved mood) compared to baseline in both hookworm treatment groups at all evaluation visits; however, longitudinal and inter-cohort analyses did not detect any significant differences over time or between groups, even when the active hookworm treatment groups were combined (Mann–Whitney test) (Table 3).
Analysis of potential confounding variables: diet and exercise habits
Participants completed regular questionnaires to record any changes in diet and exercise habits that could impact metabolic health results whilst undergoing treatment during the trial31. Analysis of the diet questionnaire (PREDIMED) revealed no significant inter-cohort differences or longitudinal changes in PREDIMED score in any treatment group (Supplementary Fig. 2A). Similarly, analysis of the exercise habits of participants by quantifying their median numbers of metabolic equivalent of tasks (METs) per week revealed no significant changes within groups from baseline and no significant differences in median absolute METs/week or changes in METs/week between groups at any time point (Supplementary Fig. 2B).
Evaluation of hookworm establishment and immune responses
Hookworm infection is associated with the presence of hookworm eggs in stool, peripheral blood eosinophilia and a type 2 cytokine response. As expected, eosinophil counts remained stable in the Placebo cohort (Fig. 2A), and faecal samples were negative for hookworm ova (Fig. 2C). In both the L3-20 and L3-40 groups, eosinophil counts peaked and were significantly elevated from baseline at 6 months (L3-20 p = 0.047, L3-40 p = 0.002, Tukey's posthoc test) but began decreasing back to normal values after 12 months (Fig. 2A). Of the 28 hookworm-treated participants, five faecal samples were unavailable for qPCR testing due to early dropout or inability to deliver a faecal sample. Twenty-one of the 23 participants (91%) tested positive for N. americanus ova at 6 months (Fig. 2C), and the two participants that tested negative still displayed robust increases in eosinophil counts (Fig. 2B). Quantification of hookworm infection intensity (hookworm eggs per gram, EPG) revealed that there was substantial variability in hookworm EPGs between hookworm-treated participants, with no clear differences in infection intensity between groups that received either 20 or 40 hookworm L3 (Fig. 2D). Analysis of serum cytokine responses in the combined hookworm cohorts revealed significantly increased levels of IL-5 at both 6 and 12 months (p = 0.0001 and p = 0.02, respectively); however levels of other type 2 or regulatory cytokines such as IL-4, IL-13 and IL-10 were not significantly elevated above baseline (Supplementary Fig. 3). Similarly, there were no significant alterations in the levels of pro-inflammatory cytokines such as IFNγ, TNF, or IL-2; however IL-17A levels were significantly reduced at 6 months after treatment (p = 0.03, Supplementary Fig. 3).
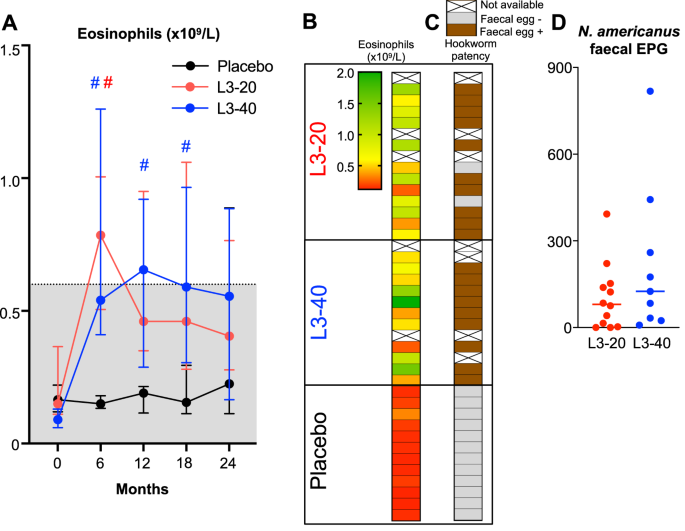
A Peripheral blood eosinophil counts (median ± IQR) at each evaluation visit, shaded area indicates normal range (Sample size for month 0, 6, 12, 18 and 24: Placebo n = 12, 12, 9, 8 and 6; L3-20 n = 13, 12, 11, 11 and 8; L3-40 n = 11, 11, 10, 8 and 8, respectively). # Indicates significantly different to 0 months; Tukey's posthoc test: (B) Heat map displaying eosinophil counts the 6 month visit (peak eosinophilia) in each participant and correlation with the (C) detection of hookworm eggs in faeces by qPCR (Hookworm patency). Some samples were unable for analysis due to dropping out prior to the 6-month visit. D Quantification of hookworm eggs per gram (EPG) in faecal samples at 6 months (median, and individual data points, L3-20 n = 12, L3-40 n = 9). Source data are provided as a Source Data File.
Metabolic outcomes: Insulin resistance (HOMA-IR)
We undertook a per-protocol analysis of secondary metabolic outcome measures to account for pre-established protocol deviations, including the Placebo participant who received hookworm treatment in error. Data collected from the 4 participants described in the Study Progression section who, at 18 or 24 months, were retrospectively discovered to have undertaken gastric sleeve surgery or began taking metformin were also excluded from the analysis. Data from one L3-20 participant whose insulin (47 mU/L), glucose (12.4 mmol/L) and HOMA-IR (26 units) values at 6 months were well beyond normal ranges and inconsistent with fasting were also excluded.
A key secondary outcome of the trial was to determine the effect of hookworm treatment versus placebo on insulin resistance, as assessed by changes in HOMA-IR. Median HOMA-IR values in the Placebo group fluctuated between improved and worsened from the baseline value of 2.2 [2.0–2.6], reaching a maximum of 2.9 [1.8–4.2] at 12 months, corresponding to a median increase of 0.8 units [−0.7 to 2.3] (Table 4 and Fig. 3A). In contrast, median HOMA-IR value in the L3-20 group was significantly lowered from the baseline value of 3.0 [2.3–3.6] to 1.8 [1.7–2.5] at 12 months (p = 0.039) and 2.1 [1.5–2.3] at 24 months (p = 0.047). Median change in HOMA-IR values in the L3-20 group was significantly different from Placebo at 12 months (p = 0.039, Kruskal–Wallis). Similar trends toward lowered HOMA-IR values were observed in the L3-40 group at 6 months (−0.5 units [−1.2 to 0.2]) and 12 months (−0.4 units [−1.4 to 0.9]); however, these changes were not statistically different from Placebo at any evaluation visit. To investigate whether improvements in HOMA-IR were correlated with increased hookworm infection intensity, we analysed changes in HOMA-IR at 6 months relative to hookworm eggs per gram (EPG). Simple linear regression analysis revealed no association between infection intensity and improvements in insulin resistance (R2 = 0.0005, p = 0.93, Supplementary Fig. 4).
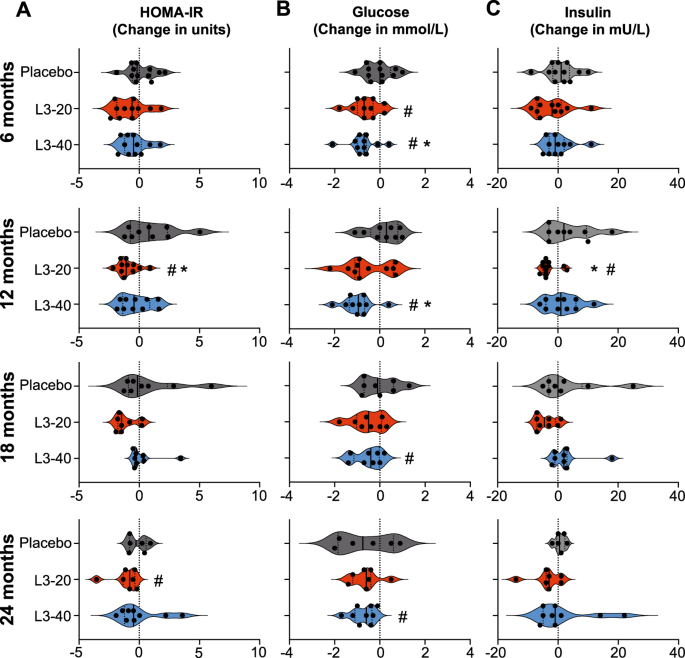
Changes in the (A) Homoeostatic model assessment of insulin resistance (HOMA-IR, units), B fasting blood glucose and (C) fasting blood insulin levels from baseline values at each 6-monthly evaluation visit. Violin plots display each individual data point, median and IQR. Dotted vertical line indicates baseline levels (0 change). *Significant difference to placebo, Kruskal–Wallis test with Dunn's multiple comparisons. #Median value significant difference to baseline, Durbin, Skillings–Mack test and Wilcoxon signed-rank test. Source data are provided as a Source Data File.
Since significance tests depend greatly on sample size, and numbers in all groups were low, we calculated the effect sizes of treatment versus control to measure the treatment effect independent of participant numbers. Effect sizes for HOMA-IR changes in the L3-20 versus Placebo group were large at 6 months (d = 0.80), 12 months (d = 1.34), 18 months (d = 1.19) and 2 years (d = 0.90). For the L3-40 group, effect sizes were small at 6 months (d = 0.48), medium at 12 months (d = 0.73), negligible at 18 months (d = 0.18), and small at 2 years (d = −0.40) (Supplementary Table 1).
Metabolic outcomes: fasting blood glucose, insulin and glycated haemoglobin
Median FBG levels (mmol/L) in the Placebo group were stable throughout and did not significantly deviate from their starting values (p = 0.605, Durbin, Skillings–Mack test) (Table 4 and Fig. 3B). In contrast, median FBG levels were reduced from baseline levels after 6 months in both the L3-20 (baseline: 5.2 [4.7–5.6] to 6 months: 4.5 [4.0–5.1]; p = 0.016) and L3-40 groups (baseline: 5.3 [4.9–5.4] to 6 months: 4.3 [4.0–5.3]; p = 0.012). Similar significant reductions in FBG were seen in the L3-40 group at 12 months (p = 0.012), 18 months (p = 0.047) and 24 months (p = 0.012) compared to baseline; however, reductions in the L3-20 group were not statistically significant at any other time point. Median changes in FBG levels in the L3-20 treatment group were not significantly different from Placebo at any time point, but changes in the L3-40 group were significantly different to Placebo at 6 months (−0.7 in L3-40 compared to 0.0 in Placebo; p = 0.027) and 12 months (−1.0 in L3-40 compared to +0.3 in Placebo; p = 0.024).
Fasting insulin levels (mU/L) were stable in the Placebo group throughout the study, ranging from a baseline of 11 [9–12] to a maximum of 12 [10–15] at 6 months (Table 4 and Fig. 3C). There were no longitudinal changes in insulin levels in the L3-40 group at any time point and no significant differences compared to Placebo. Insulin levels in the L3-20 group were consistently lowered from the baseline level of 13 [12–16] to 10 [9–14] at 12 months (p = 0.031 compared to baseline), with reductions from baseline values reaching statistical significance compared to Placebo at 12 months (−4.0 in L3-20 compared to +2.0 in Placebo; p = 0.02).
Levels of glycated haemoglobin (HbA1cIFCC, mmol/mol) displayed an upward trend at all evaluation visits compared to baseline in the Placebo group, ranging from a baseline value of 32 [30–33] mmol/mol to a maximum of 35 [33–37] at 2 years (Supplementary Table 2). Values in the L3-20 group were stable near the baseline value of 33 [30–35] throughout, while values in the L3-40 group experienced similar upward trends to the Placebo group, with values significantly higher than baseline at 18 months (p = 0.031).
Secondary metabolic outcomes: body mass and blood lipid profile
Median body mass and Body Mass Index (BMI) in the Placebo group remained stable throughout (Table 5, Fig. 4 and Supplementary Fig. 5). While there were no statistically significant differences in body mass or BMI in the L3-20 or L3-40 groups compared to Placebo (Table 5), body mass and BMI in the L3-20 group tended to be lower than their baseline values at all evaluation visits, with significant reductions in body mass and BMI in the L3-20 group at 18 months (p = 0.031 for body mass, p = 0.016 for BMI) and 24 months (p = 0.031 for body mass and p = 0.016 BMI). This corresponded to a median reduction in body mass of approximately 5 kg at both time points in the L3-20 group (Table 5 and Fig. 4) and a reduction in BMI of 2.2 units and 2.4 units at 18 months and 2 years, respectively (Table 5 and Supplementary Fig. 5). No significant longitudinal changes in body mass or BMI were evident in the L3-40 group.
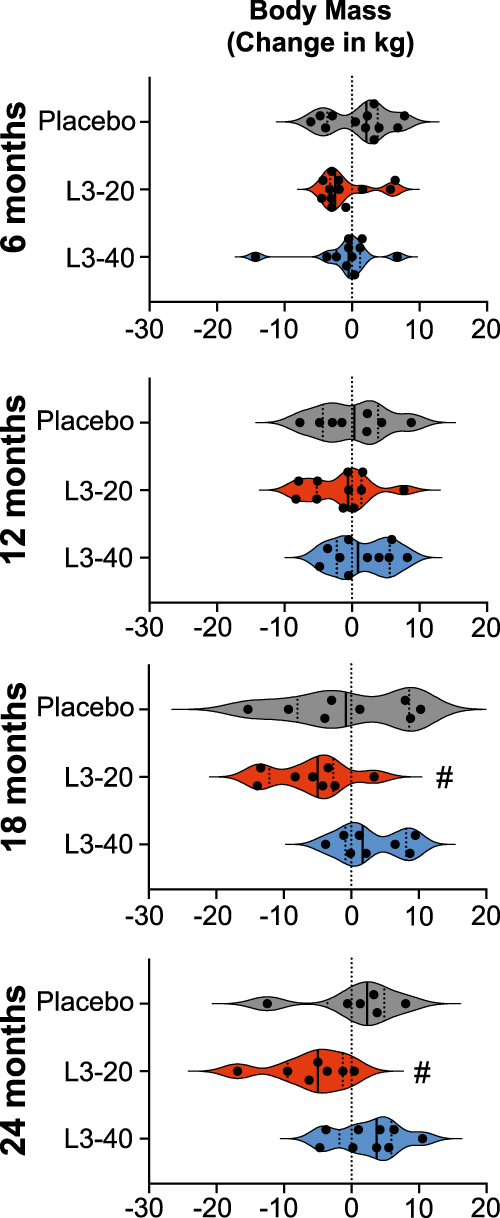
Changes in participant's body mass (kg) from baseline values at each 6-monthly evaluation visit. Violin plots display each individual data point, median and IQR. Dotted vertical line indicates baseline levels (0 change). #Median value significant difference to baseline, Durbin, Skillings-Mack test and Wilcoxon signed-rank test: Source data are provided as a Source Data File.
Analysis of blood lipid profile revealed that median levels of total cholesterol, triglycerides, high-density lipoprotein, low-density lipoprotein and total cholesterol/HDL ratio remained relatively stable in the Placebo group at all time points, with only a statistically significant reduction in LDL at 12 months (p = 0.016) and 18 months (p = 0.023) (Supplementary Tables 3 and 4). In both the L3-20 and L3-40 groups, there were no longitudinal changes in any of these parameters compared to baseline and no significantly different changes compared to Placebo other than elevated LDL (p = 0.019) and total cholesterol (p = 0.038) at 18 months in the L3-40 group compared to Placebo (Supplementary Tables 3 and 4)
Discussion
Over recent decades, helminth infection has emerged as a potential approach for treating allergic and autoimmune disorders, as well as metabolic disorders such as Metabolic Syndrome and type 2 diabetes15,21,27. Until now, a potential supportive role for worms in metabolic health has relied on animal studies and human cross-sectional or deworming studies that could not infer causality. The present study provides human clinical trial evidence supporting the potential beneficial effect of helminth infection in metabolic disease. Infection with low doses of hookworms caused significantly reduced measures of glucose homoeostasis (lowered HOMA-IR and fasting blood glucose) compared to pre-infection and Placebo treatment, which was associated with modest body mass reductions. Regular monitoring of diet and physical activity habits revealed no consistent changes that could have contributed alone to improved insulin resistance. While the study was relatively small and needs to be validated by larger follow-up studies, the results provide proof of principle that hookworms and/or the biological changes they invoke in their human hosts are a safe and potentially beneficial intervention for improving determinants of metabolic health.
The primary outcome of this Phase Ib study was to determine the safety and tolerability of hookworm infection in people at risk of developing T2D. While hookworm infection was associated with a higher incidence of gastrointestinal AEs, these were anticipated during the time that hookworms established in the gut30 and were typically mild-moderate and resolving. Three of the 28 hookworm-treated participants displayed GI symptoms that warranted deworming, and symptoms resolved promptly in two. The third did not improve after deworming, suggesting their symptoms were unrelated to hookworm infection. Overall, the safety profile of hookworm treatment in people at risk of T2D is similar to that in other diseases30.
In the current study, hookworm infection was associated with improved insulin resistance, consistent with previous mouse or natural human helminth infection studies7,21,32. Lowered HOMA-IR was most apparent in the group that received 20 hookworms and was most pronounced at 18 months, with a reduction in median HOMA-IR from 3.0 units at baseline (consistent with pre-diabetic insulin resistance) to 1.6 units at 18 months (a healthy level). The large Cohen's d effect sizes in the L3-20 group highlight the statistical and clinical significance of this sustained improvement in metabolic health. Interestingly, the improvements in HOMA-IR in the group that received 40 worms were less dramatic, despite similar trends in reduced HOMA-IR at 6 and 12 months. Both the L3-20 and L3-40 groups showed similar reductions in fasting blood glucose compared to Placebo throughout the study, but only the L3-20 group displayed sustained reductions in insulin. By the later stages of the study, all results from the L3-40 group were comparable to Placebo. Notably, we did not detect consistently higher degrees of hookworm infection intensity (hookworm EPGs) or significantly stronger eosinophil responses with the higher dose of worms, and correlation analyses did not show a significant association between higher worm doses and faecal EPGs with greater improvements in HOMA-IR. Clearly, larger clinical trials are required to clarify the optimal dose of hookworms. One factor that may partially explain why participants in the L3-20 cohort responded better to treatment was that pre-trial median age and HOMA-IR were higher; hence there was greater potential for improvements. Future clinical trials designed to demonstrate efficacy should stratify participants based on high and low baseline HOMA-IR.
In conversations with potential participants during recruitment and screening, it was evident that a powerful motivator to enrol was the prospect of body mass reductions, as documented in mouse20,22,24 or natural human helminth infection studies7,24,32,33. We noted modest reductions in body mass and BMI in the L3-20 group; however, body mass reductions were not consistent for all hookworm-treated participants, possibly due to the relatively low worm burdens compared to those seen in animal studies or natural infections. This caused disappointment for some people, who then elected to pursue gastric sleeve surgery despite improvements in HOMA-IR. Most participants were less concerned and continued with unabated enthusiasm. Bar one, all hookworm-treated participants that completed the study opted to retain their worms, and the sole person who dewormed did so in preparation for a medical procedure.
Interestingly, hookworm infection did not show significant improvements in blood lipid profiles, in contrast to what may have been expected based on previous studies9,10,13,24,33. A potential explanation could lie in the different helminth species used in the current trial. Previous studies noting improved blood lipid markers included cross-sectional and deworming studies of infections with multiple soil-transmitted helminths33 and previous and current schistosomiasis9,10,13,24 but not hookworm infection alone. Results from a 2019 systematic review and meta-analysis suggested that different helminth species may have different efficacy in altering lipid and glucose homoeostasis15. The authors postulated that the liver-specific residence of Schistosoma spp. compared to intestinal helminths could facilitate greater metabolic improvements in schistosomiasis. Future helminth challenge studies such as ours that instead use single-sex infections with schistosome parasites34 may validate this hypothesis.
The study had several limitations, with the major shortcoming being the small sample sizes that limited our ability to make firm conclusions. This was further curbed by the long duration of the study and attrition of participants in all groups after the 12-month time point. Since T2D takes many years to manifest, future studies will need to follow up with participants for longer periods. Ideally, this would be combined with repeated doses of hookworms to maintain a chronic infection and monitoring of the associated immune response. Such studies could include a deworming arm to determine if an active hookworm infection is required for longer-term benefits and could use HbA1c IFCC as a longer-term primary outcome measure of improved glycaemic control. Additionally, participant selection bias limited the generalisability of our findings. Most participants were of Caucasian descent, and it is unclear if different populations, such as people of Asian descent or Australian First Nations people, who disproportionately suffer from T2D35, would experience similar improvements. Further, our qPCR methods for quantifying hookworm infection intensity (EPGs) may not accurately reflect the true level of hookworm burden. Our qPCR assay was based on the quantification of non-embryonated eggs, and in our study, faecal samples provided by participants were not always immediately frozen, potentially allowing some eggs to embryonate. This would cause the levels of parasite DNA to increase, resulting in the qPCR overestimating parasite egg burdens. Future studies should use ethanol fixation, which would allow for better standardisation of methods for determining hookworm infection intensities. Lastly, within the scope of this study, we could not attain a mechanistic understanding of how and why hookworm infection caused improvements in insulin resistance. It remains conceivable that improvements in insulin resistance could have been a direct consequence of reduced body mass after hookworm treatment; however significant reductions in body mass were not observed until after significant improvements in HOMA-IR were seen. Nevertheless, future studies that are designed to demonstrate efficacy should attempt to explore the potential kinetic relationships between hookworm-mediated body mass reductions and changes in insulin resistance. Regarding potential direct mechanisms of hookworm-mediated improvements in metabolic health; type 2 immune responses and eosinophils are known to counteract detrimental pro-inflammatory cytokine responses and positively influence metabolism20,36, and we did observe consistent elevations in circulating eosinophils and type 2 cytokines such as IL-5, so it remains plausible that they contributed to stimulating this pathway. However, we did not observe any evidence that hookworm infection supressed systemic pro-inflammatory cytokine levels other than modest and transient reductions in IL-17A. It should be noted however that the time points at which we assessed changes in immune profiles (6 and 12 months) were likely too late to detect the more acute changes that would have occurred as the worms established in the human host11. Better understanding of the beneficial biological effects of hookworms in the context of metabolic syndrome may identify novel therapeutic strategies that could mimic the actions of the live hookworm (e.g. immune-modifying or microbiome therapies) or may pinpoint factors that are excreted/secreted by hookworms that could be produced as novel biologic therapies37.
In conclusion, the hygiene hypothesis8,12 provides...
Comments
Post a Comment